Baohuoside I Inhibits Benzo(a)Pyrene-Induced Metastasis in A549 Lung Cancer Cells by Modulating STAT3 and EMT
Baohuoside I Inhibits Benzo(a)Pyrene-Induced Metastasis in A549 Lung Cancer Cells by Modulating STAT3 and EMT
Muhammad Khan1,*, Amara Maryam2, Hafiz Abdullah Shakir1, Javed Iqbal Qazi1 and Yongming Li3,*
1Department of Zoology, University of the Punjab, Quaid-i-Azam Campus, Lahore 54590, Pakistan
2College of Basic Medical Sciences, Dalian Medical University, Dalian, Liaoning116044, P.R. China
3Institute of Traditional Chinese Medicine, Nanjing University of Chinese Medicine, Nanjing 210023, P.R. China
ABSTRACT
Benzo(a)pyrene (BaP), a major component of cigarette smoke, has been found to be a potent human carcinogen. Recently, it has been shown to induce lung cancer metastasis. In the present study, we found for the first time that Baohuoside I (BHS-1), a natural flavonol glycoside inhibits BaP-induced A549 lung cancer metastasis by modulating the expressions of p-STAT3, COX-2, MMP-2, MMP-9, E-cadherin and N-cadherin. Moreover, we found that chronic BaP exposure promoted migration without enhancing the proliferation of cells and BHS-I was equally toxic to both BaP-treated and untreated A549 cells. Taken together, the data of present study indicate that BHS-I not only inhibits metastasis but also induces cell death in BaP-treated A549 cells. Therefore, BHS-I may become a potential lead compound for treatment of lung adenocarcinoma.
Article Information
Received 13 August 2018
Revised 23 September 2018
Accepted 22 October 2018
Available online 31 October 2018
Authors’ Contribution
MK and YL designed the study. AM performed the experimental work. MK analyzed the data and wrote the paper. HAS and JIQ reviewed the article for language mistakes.
Key words
Benzo(a)Pyrene, STAT3, EMT, Lung cancer metastasis, Baohuoside I.
DOI: http://dx.doi.org/10.17582/journal.pjz/2018.50.6.2357.2365
* Corresponding authors: [email protected];
0030-9923/2018/0006-2357 $ 9.00/0
Copyright 2018 Zoological Society of Pakistan
Introduction
Lung cancer is one of the most common cancers both in term of prevalence and mortality worldwide (Roviello, 2015; Maryam et al., 2017; Gulzar et al., 2018). Approximately 1.4 million deaths occur per annum worldwide due to lung cancer, of which 0.6 million deaths occur only in China (She et al., 2013). Smoking has been considered as the major risk factor which is responsible for about 90% cases of lung cancer (Kamaraj et al., 2010). Benzo[a]Pyrene (BaP), a highly carcinogenic polycyclic aromatic hydrocarbon, is widely found in tobacco smoke, charcoal-grilled food, contaminated water and engine exhaust (Hung et al., 2015; Ba et al., 2015). It gets into human body mainly through inhalation and ingestion. Inhalation of BaP induces lung cancer while ingestion results in development of tumor in various organs including liver, gastric, lungs and mammary glands (Ba et al., 2015; Benford et al., 2010). It has now been categorized as Human Group 1 carcinogen by the International Agency for Research on Cancer (Ba et al., 2015). Recent research indicates that BaP promotes invasion and metastasis of lung cancer cells in vitro and in vivo by inducing the expressions of Twist (Wang et al., 2015), cyclooxygenase-2 (COX-2), matrix metalloproteinases (MMP-2 & -9) (Kamaraj et al., 2010) and epithelial-mesenchymal transition (EMT) related genes (Hung et al., 2015).
Natural products are excellent source of biologically active molecules against various ailments. Plants have a long history of use in folk medicines. Plants’ secondary metabolites such as alkaloids, terpenes and polyphenoles have been shown to inhibit cancer progression by interfering with multiple mechanisms which are considered as the key mediators of various human cancers (Khan et al., 2015, 2016). Flavonoids are polyphenolic compounds, widely distributed in plants and exist as aglycone or glycosides. Modern research has shown that flavonoids are the potent anticancer compounds. Baohuoside I (BHS-1), a flavonol glycoside also termed as Icariside II, is one of the most important constituents of Herba epimedii and Cortex periplocae which are traditional Chinese medicines used to treat various ailments including cancer, inflammation, and neurological functions. BHS-I has been reported to exhibit anticancer activity against various human cancer cell lines through multiple mechanisms (Khan et al., 2015).
In the present study, we found for the first time that BHS-I holds the promise to inhibit BaP-induced A549 lung cancer metastasis. The anti-metastatic activity of BHS-I was found to be associated with inhibition of STAT3 activation at tyrosine705 (Tyr705), decreased expression of Cox-2, MMP-2, MMP-9, and N-cadherin and increased expression of E-cadherin.
Materials and Methods
Reagents and antibodies
BHS-I (purity >98%) was obtained from Tauto Biotech. Co., Ltd. (Shanghai, China). The chemical structure of BHS-I is shown in Figure 1A. BaP, propidium iodide (PI), calcein acetoxymethylester (Calcein AM), dimethyl sulfoxide (DMSO), [3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide] (MTT), Dulbecco’s Modified Eagle’s Medium (DMEM), fetal bovine serum (FBS), penicillin and streptomycin were purchased from Sigma (Beijing, China). Antibodies specific to p-STAT3, STAT3, COX-2, MMP-2, MMP-9 were purchased from Cell Signaling Technology (Shanghai, China) while antibodies specific to E-cadherin, N-cadherin and Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) were purchased from Proteintech (Wuhan, Hubei, China). Horseradish peroxidase-conjugated secondary antibodies (goat-anti-rabbit, goat-anti-mouse) were purchased from Santa Cruz (Beijing, China).
Cell culture and treatments
Human non-small cell lung cancer A549 cells were obtained from American Type Culture Collection (ATCC) and maintained in DMEM supplemented with 10% FBS, 100 units/mL penicillin and 100 μg/mL streptomycin at 37°C with 5% CO2 in humidified atmosphere. A549 cells were treated with 1μM BaP dissolved in DMSO for 4 weeks with a final DMSO concentration of 0.5%. The culture medium containing 1μM BaP was exchanged twice a week. BaP-treated A549 cells were designated as A549/B. A549/B cells were cultured in medium containing 1μM BaP for various experiments. To evaluate the anti-metastatic effect of BHS-1, cells were incubated with 15μM BHS-1 which was found to be non-toxic concentration. A549 cells were treated only with 0.5% DMSO.
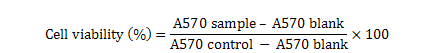
Determination of cell viability
The effect of BaP on cell viability was determined by MTT assay as described by us previously (Khan et al., 2012a). Briefly A549 and A549/B cells were cultured in 96 well plate in triplicate in the presence or absence of 15 and 30 μM BHS-I for 24 h. Following treatment, 10 μL MTT (5 mg/mL) reagent was added and cells were further incubated at 37°C for 4 h. Subsequently medium was replaced and 150 μL DMSO was added to dissolve farmazan crystals and absorbance was measured at 570 nm by Synergy new microplate reader, BioTek. The percentage of cell viability was calculated as follows:
Live / dead assay
The effect of BHS-I on A549 and A549/B cells death was evaluated by live/dead assay as described previously (Khan et al., 2012b). A549 and A549/B cells were cultured in 6 well plates and treated with IC50 (30 μM) of BHS-I which was determined through preliminary experiments with reference to the previous report (Song et al., 2012) for 24 h. Following treatment, the floating and adherent cells were collected, washed with phosphate buffered saline (PBS) twice and incubated in PBS solution containing 2 μM calcein AM and 4 μM PI in the dark for 20 min at room temperature. The cells were washed with PBS twice and re-suspended in PBS solution. The cells were analyzed for the fluorescence of calcein and PI by fluorescence microscope (Leica, DMI 4000B). Finally 100 cells were counted microscopically from 3 different areas for the percentage of live and dead cells.
In vitro cell migration assay
In vitro cell migration was assessed by wound healing and transwell chamber assays. For wound healing assay, A549 and A549/B cells were cultured in 12 well plates for 24 h. The cells were then scraped with a sterile 200μL tip and washed with PBS to remove cellular debris. Fresh medium containing DMSO or BaP was added to respective wells. The cells were further incubated for another 24 h in the presence or absence of 15μM (non-toxic concentration) BHS-I. The movement of cells in scratched area was photographed by using Leica, DMIL LED inverted microscope equipped with a digital system at 0 and 24 h.
For transwell chambers, cells were cultured and treated in a similar way for 24 h. Finally 1 × 105 cells in 200 μLof medium with 1% FBS were seeded in the upper transwell insert chamber containing a polycarbonate filter (6.5-mm diameter, 8-μm pores; Corning Costar, Corning, NY, USA). 600 μL DMEM with 10%FBS was added to the lower chamber and cells were further incubated for 24 h. The cells on the upper surface of membrane were removed carefully by cotton swabs. The cells on the lower surface was fixed with 4% paraformaldehyde, stained with crystal violet and observed under microscope. To quantify the migration ability of cells, three areas were randomly selected from each group and the number of cells was counted microscopically.
Western blotting
A549 and A549/B cells were treated with or without BHS-1 (15μM) for 24 h. Proteins were isolated from cells as described previously (Khan et al., 2012a) Protein concentrations were determined using enhanced BCA protein Assay kit (Beyotime, Nanjing, China) by spectrophotometer (Synergy new microplate reader, BioTek). Equal amount of proteins were separated on 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto a polyvinylidine difluoride (PVDF) membrane. The membranes were blocked with 5% non-fat milk for 1 h at room temperature, washed three times with Tris-buffered saline with Tween-20 (TBST) and incubated with p-STAT3 (1:1000), STAT3 (1:1000), COX-2 (1:1000), MMP-2 (1:1000), MMP-9 (1:1000), N-Cadherin (1:500), E-Cadherin (1:500) and GAPDH (1:1000) antibodies overnight at 4°C. After washing three time with TBST, the membrane were incubated with horseradish peroxidase-conjugated goat anti-rabbit or -mouse IgG secondary antibodies for 1 h at room temperature. After washing with TBST, signals were detected using ECL plus chemiluminescence kit by DNR bioimaging system MicroChemi 4.2. GAPDH was used as loading control in every individual blot.
Statistical analysis
Data are expressed as mean±SEM of three different experiments and statistically compared with control group or within the groups using one way ANOVA followed by Tukey’s Multiple Comparison Test and P < 0.05 was considered statistically significant.
Results
Effect of BaP on cell proliferation
The effect of BaP on A549 cell proliferation was determined by MTT assay. In order to investigate the effect of long term BaP treatment on cell proliferation, A549/B cells were exposed to 1μM BaP for 4 weeks and their proliferation was compared with DMSO treated A549 cells. No significant difference in growth rate of A549/B and A549 cells was observed as shown in Figure 1B. Moreover, 1μM BaP treatment did not induce any morphological change or cytotoxic effect in A549/B cells.
BHS-I inhibits growth and induces cell death both in A549 and A549/B cells
Cigarette smoking has been shown to confer drug resistance in lung cancer patients (Vu et al., 2016). Therefore, the cytotoxic effect of BHS-I on A549 and A549/B cells were evaluated by MTT and live/dead assays. For this, A549 and A549/B cells were cultured in medium containing DMSO and BaP for 24 h. The cells were then treated with 30μM BHS-I for 24 h and cell viability was determined by MTT and live/dead assays. The data demonstrated that BHS-I was equally toxic to both A549 and A549/B cells indicating that BaP did not enhance anti-apoptotic potential of A549/B cells. The results have been shown in Figure 1B and C.
BHS-I inhibits BaP-induced migration in A549/B cells
BaP has been reported to enhance migration in A549 lung cancer cells (Wang et al., 2015). In agreement with previous reports, long term exposure of cells to relatively low dose of BaP enhanced migration of A549/B cells as assessed by wound healing and transwell migration assays. Next we wonder if BaP-induced migration could be inhibited by BHS-1. The data showed that BHS-1 significantly inhibited the migration ability of A549/B cells as evident by wound healing and transwell migration assays (Fig. 2).
BHS-I inhibits BaP-induced STAT3 activation in A549/B cells
Signal transducer and activator of transcription 3 (STAT3) is a cytoplasmic transcription factor which has been implicated in tumor cells proliferation, survival, angiogenesis, invasion, migration and epithelial to mesenchymal transition (EMT) (Grivennikov and Karin 2010; Khan et al., 2015). Therefore, we measured the activation of STAT3 at Tyr705 in A549/B cells by Western blot. The data showed that BaP treatment activated STAT3 by inducing phosphorylation at tyrosine 705 (Y705) in A549/B cells. Next we asked if BaP-induced phosphorylation of STAT3 could be inhibited by BHS-I. As shown in Figure 3, BHS-I reversed BaP-induced phosphorylation of STAT3 in A549/B cells.
BHS-I decreases BaP-induced COX-2 expression in A549/B cells
Cox-2, a powerful mediator of cancer invasion and metastasis has been reported to overexpress in about 85% of lung cancer cases (Sandler and Dubinett, 2004; Kamaraj et al., 2010). Here we found that BaP significantly increased the expression of COX-2 in A549/B cells compared to DMSO treated A549 cells. This BaP-mediated increased expression of COX-2 was effectively inhibited by BHS-I as shown in Figure 4.
BHS-I decreases BaP-induced MMP-2 and -9 expressions in A549/B cells
MMP-2 and MMP-9 are matrix metalloproteinases that play vital role in cancer invasion and metastasis by degrading extracellular matrix (ECM) components (Khan et al., 2016). COX-2 expression has been positively associated with MMP-2 and -9 expressions (Kamaraj et al., 2010). Therefore, we measured the expression of MMP-2 and -9 in A549 cells. That data showed that BaP treatment enhanced the expression of MMP-2 and -9 in A549/B cells compared to DMSO-treated A549 cells and this increased expression was significantly suppressed by BHS-I (Fig. 4).
BHS-I inhibits BaP-induced EMT in A549/B cells
The epithelial-mesenchymal transition (EMT) is a crucial event of the invasion-metastasis cascade (Palmirotta et al., 2016). EMT is a cellular phenomenon in which epithelial markers such as E-cadherin are down-regulated while mesenchymal markers such as N-cadherin and vimentin are up-regulated (Vu et al., 2016). Therefore, we measured the expression of E-cadherin and N-cadherin in A549 cells. The data demonstrated that BaP treatment decreased the expression of E-cadherin and increased the expression of N-cadhern in A549/B cells. As shown in Figure 5, BaP-induced EMT was effectively inhibited by BHS-I.
Discussion
Metastasis, the hallmark of malignant tumors is responsible for about 90% of cancer patient deaths. It is believed to be the most challenging obstacle to successful chemotherapy of cancer patients (Jiang et al., 2011; Khan et al., 2016). The relationship between cigarette smoking and poor prognosis of lung cancer has now been well established. BaP, one of the major components of cigarette smoking, has recently been reported to induce lung cancer metastasis (Kamaraj et al., 2010; Huang et al., 2015; Wang et al., 2015). The present study was designed to reverse the BaP-induced metastatic potential of A549 lung cancer cells by natural compounds. For this, we have established A549/B cell line from parental A549 cell line by chronic exposure to BaP for 4 weeks. A549/B cells were found to share similar growth rate and morphological characteristics with parental cells however, were found to exhibit significantly higher migration rate compared to parental cells. Moreover, we found that BHS-1, a natural flavonol glycoside could effectively inhibit BaP-induced metastasis in A549/B cells. To characterize in detail the molecular mechanism by which BHS-1 inhibits BaP-induced migration of A549/B cells, we measured the expressions of various proteins involved in cancer metastasis in both parental A549 and A549/B cells in the presence or absence of BHS-1.
Several lines of evidence suggest that inflammation is one of the major players of cancer development and metastasis (Bremnes et al., 2011; Wang et al., 2012). STAT3, a major mediator of inflammation has been reported to overexpress in several cancer types. Accumulating evidence has suggested that aberrant expression and activation of STAT3 has been implicated in lung cancer progression, drug resistance and metastasis (Khan et al., 2015; Lee et al., 2015; Nan et al., 2014). Other research reports indicate that cigarette smoking can induce STAT3 activation and inflammation in human bronchial epithelial cells (Liu, 2007). Impressed by the above mentioned research reports, we were interested to know whether BaP, a major component of cigarette smoke could induce STAT3 activation in A549/B cells. Our data demonstrated that BaP increased phosphorylation of STAT3 which was effectively reversed by BHS-1. Our finding are further supported by previous research reports where BHS-1 has been shown to inhibits STAT3 activation in A375 human melanoma, A431 human epidermoid carcinoma,U266 multiple myeloma and U937 acute myeloid leukemia cells (Khan et al., 2015).
Once activated, STAT3 translocates into nucleus where it controls the expression of target genes important for cell proliferation, survival, drug resistance, angiogenesis, invasion and metastasis (Yue and Turkson, 2009). COX-2, one of the STAT3 downstream transcription factors and main mediator of inflammation, over-expresses in a wide range of human cancers and is closely associated with inflammation, angiogenesis and cancer metastasis (Khan et al., 2015). Here we found that BaP induced the expression of COX-2 in A549/B cells while BHS-1 suppressed the induced expression of COX-2.
Matrix metalloproteinases (MMPs) are a family of zinc binding proteolytic enzymes that play fundamental role in normal physiological processes such as embryonic development, wound healing, angiogenesis as well as in several pathological processes such as carcinogenesis (Kim et al., 2008). Because of their ability to degrade components of extracellular matrix (ECM), they are implicated in invasion and metastasis of wide range of human cancers (Pietruszewska et al., 2016). Among various members of MMPs, MMP-2 (Gelatinase-A) and -9 (Gelatinase-B) consistently express in malignant tissues and play vital role in cancer invasion and metastasis (Kamaraj et al., 2010). In the present study, we sought to clarify if the expression of MMP-2 and -9 is modulated during BaP-induced metastasis of lung cancer cells. We found higher expression of MMP-2 and -9 in A549/B cells compared to A549 cells. This BaP-mediated expression of MMP-2 and -9 was attenuated by supplementation of BHS-1.
EMT is a phenomenon in which epithelial cells lose their polarity and ultimately acquire mesenchymal phenotype. During EMT, expression of epithelial markers such as E-cadherin decreases and expression of mesenchymal markers such as N-cadherin and vimentin increases. EMT plays vital role in embryonic development, wound healing and cancer progression. Among EMT markers, down-regulation of E-cadherin has been considered as the hallmark of EMT (Palmirotta et al., 2016; Vu et al., 2016). EMT is a crucial event of the invasion-metastasis cascade. Epidemiological studies have shown that in smokers higher expressions of mesenchymal markers and decreased expression of epithelial markers have been detected compared to non-smokers (Milara et al., 2013; Sohal et al., 2010; Vu et al., 2016). Very recently Li et al. (2016) have shown that in vitro exposure of cigarette smoke extract could promote EMT in lung cancer cells. Moreover, increased EMT has been detected in patients of chronic obstructive pulmonary disease which is mainly caused by smoking. In line with the previous findings, here we found that BaP, a component of cigarette smoke increased the expression of N-cadherin and decreased the expression of E-cadherin in lung cancer cells. This BaP-induced EMT was effectively inhibited by BHS-1.
Conclusion
In conclusion, the findings of our study indicate that BaP might hold the answer at least to some extent to the adverse effects of smoking particularly in poor prognosis of lung cancer patients. Moreover, our data showed that BHS-1 effectively inhibits BaP-induced A549 lung cancer cells metastasis in vitro by STAT3 inactivation, decreased expression of COX-2, MMP-2, and -9 and inhibition of EMT. Thus BHS-1 might be developed into a novel anti-cancer and anti-metastatic agent for lung adenocarcinoma.
Statement of conflict of interest
The authors declare no conflict of interest.
References
Ba, Q., Li, J., Huang, C., Qiu, H., Chu, R., Zhang, W., Xie, D., Wu, Y. and Wang, H., 2015. Effects of benzo[a]pyrene exposure on human hepatocellular carcinoma cell angiogenesis, metastasis, and NF-kappaB signaling. Environ. Hlth. Perspect., 123: 246-254. https://doi.org/10.1289/ehp.1408524
Benford, D., Dinovi, M. and Setzer, R.W., 2010. Application of the margin-of-exposure (MoE) approach to substances in food that are genotoxic and carcinogenic e.g.: benzo[a]pyrene and polycyclic aromatic hydrocarbons. Fd. Chem. Toxicol., 48(Suppl-1): S42-48. https://doi.org/10.1016/j.fct.2009.09.039
Bremnes, R.M., Al-Shibli, K., Donnem, T., Sirera, R., Al-Saad, S., Andersen, S., Stenvold, H., Camps, C. and Busund, L.T., 2011. The role of tumor-infiltrating immune cells and chronic inflammation at the tumor site on cancer development, progression, and prognosis: emphasis on non-small cell lung cancer. J. Thorac. Oncol., 6: 824-833. https://doi.org/10.1097/JTO.0b013e3181f8a1bd
Grivennikov, S.I. and Karin, M., 2010. Dangerous liaisons: STAT3 and NF-kappaB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev., 21: 11-19. https://doi.org/10.1016/j.cytogfr.2009.11.005
Gulzar, A., Mahmud, T., Munir, R. and Anjum, A., 2018. Anti-cancerous and anti-inflammatory activities of some novel schiff bases derived from 2-[(1,3-benzothiazol-2-yl)sulfanyl]-N-[4-(hydrazinecarbonyl)phenyl]acetamide. Pakistan J. Zool., 50: 1003-1009. http://dx.doi.org/10.17582/journal.pjz/2018.50.3.1003.1009
Hung, J.Y., Chang, W.A., Tsai, Y.M., Hsu, Y.L., Chiang, H.H., Chou, S.H., Huang, M.S. and Kuo, P.L., 2015. Tricetin, a dietary flavonoid, suppresses benzo(a)pyrene induced human non-small cell lung cancer bone metastasis. Int. J. Oncol., 46: 1985-1993. https://doi.org/10.3892/ijo.2015.2915
Jiang, Y.L. and Liu, Z.P., 2011. Natural products as anti-invasive and anti-metastatic agents. Curr. Med. Chem., 18: 808-829. https://doi.org/10.2174/092986711794927711
Kamaraj, S., Anandakumar, P., Jagan, S., Ramakrishnan, G. and Devaki, T., 2010. Modulatory effect of hesperidin on benzo(a)pyrene induced experimental lung carcinogenesis with reference to COX-2, MMP-2 and MMP-9. Eur. J. Pharmacol., 649: 320-327. https://doi.org/10.1016/j.ejphar.2010.09.017
Khan, M., Ding, C., Rasul, A., Yi, F., Li, T., Gao, H., Gao, R., Zhong, L., Zhang, K., Fang, X. and Ma, T., 2012a. Isoalantolactone induces reactive oxygen species mediated apoptosis in pancreatic carcinoma PANC-1 cells. Int. J. biol. Sci., 8: 533-547. https://doi.org/10.7150/ijbs.3753
Khan, M., Yi, F., Rasul, A., Li, T., Wang, N., Gao, H., Gao, R. and Ma, T., 2012b. Alantolactone induces apoptosis in glioblastoma cells via GSH depletion, ROS generation, and mitochondrial dysfunction. Int. Union Biochem. mol. Biol. Life, 64: 783-794.
Khan, M., Maryam, A., Qazi, J.I. and Ma, T., 2015. Targeting apoptosis and multiple signaling pathways with icariside II in cancer cells. Int. J. biol. Sci., 11: 1100-1112. https://doi.org/10.7150/ijbs.11595
Khan, M., Maryam, A., Zhang, H., Mehmood, T. and Ma, T., 2016. Killing cancer with platycodin D through multiple mechanisms. J. Cell. mol. Med., 20: 389-402. https://doi.org/10.1111/jcmm.12749
Maryam, A., Mehmood, T., Zhang, H., Li, Y., Khan, M., Ma, T., 2017. Alantolactone induces apoptosis, promotes STAT3 glutathionylation and enhances chemo-sensitivity of A549 lung adencarcinoma cells to doxorubicin via oxidative stress. Scient. Rep., 7: 6242. https://doi.org/10.1038/s41598-017-06535-y
Khan, S., Shukla, S., Sinha, S., Lakra, A.D., Bora, H.K. and Meeran, S. M., 2015. Centchroman suppresses breast cancer metastasis by reversing epithelial-mesenchymal transition via down regulation of HER2/ERK1/2/MMP-9 signaling. Int. J. Biochem. Cell Biol., 58: 1-16. https://doi.org/10.1016/j.biocel.2014.10.028
Kim, S., Kim, Y., Kim, J.E., Cho, K.H. and Chung, J.H., 2008. Berberine inhibits TPA-induced MMP-9 and IL-6 expression in normal human keratinocytes. Phytomedicine, 15: 340-347. https://doi.org/10.1016/j.phymed.2007.09.011
Lee, J.H., Kim, C., Sethi, G. and Ahn, K.S., 2015. Brassinin inhibits STAT3 signaling pathway through modulation of PIAS-3 and SOCS-3 expression and sensitizes human lung cancer xenograft in nude mice to paclitaxel. Oncotarget, 6: 6386-6405. https://doi.org/10.18632/oncotarget.3443
Li, D., Zhang, L., Zhou, J. and Chen, H., 2016. Cigarette smoke extract exposure induces EGFR-TKI resistance in EGFR-mutated NSCLC via mediating SRC activation and EMT. Lung Cancer, 93: 35-42. https://doi.org/10.1016/j.lungcan.2015.12.007
Liu, X., 2007. STAT3 activation inhibits human bronchial epithelial cell apoptosis in response to cigarette smoke exposure. Biochem. biophys. Res. Commun., 353: 121-126. https://doi.org/10.1016/j.bbrc.2006.11.147
Milara, J., Peiro, T., Serrano, A. and Cortijo, J., 2013. Epithelial to mesenchymal transition is increased in patients with COPD and induced by cigarette smoke. Thorax, 68: 410-420. https://doi.org/10.1136/thoraxjnl-2012-201761
Nan, J., Du, Y., Chen, X., Bai, Q., Wang, Y., Zhang, X., Zhu, N., Zhang, J., Hou, J., Wang, Q. and Yang, J., 2014. TPCA-1 is a direct dual inhibitor of STAT3 and NF-kappaB and regresses mutant EGFR-associated human non-small cell lung cancers. Mol. Cancer Ther., 13: 617-629. https://doi.org/10.1158/1535-7163.MCT-13-0464
Palmirotta, R., Cives, M., Della-Morte, D., Capuani, B., Lauro, D., Guadagni, F. and Silvestris, F., 2016. Sirtuins and cancer: Role in the epithelial-mesenchymal transition. Oxid. Med. Cell. Longev., 2016: Article ID 3031459. https://doi.org/10.1155/2016/3031459
Pietruszewska, W., Bojanowska-Pozniak, K. and Kobos, J., 2016. Matrix metalloproteinases MMP1, MMP2, MMP9 and their tissue inhibitors TIMP1, TIMP2, TIMP3 in head and neck cancer: An immunohistochemical study. Otolaryngol. Pol., 70: 32-43. https://doi.org/10.5604/00306657.1202546
Roviello, G., 2015. The distinctive nature of adenocarcinoma of the lung. Oncol. Targets Ther., 8: 2399-2406. https://doi.org/10.2147/OTT.S89225
Sandler, A.B. and Dubinett, S.M., 2004. COX-2 inhibition and lung cancer. Semin. Oncol., 31(2 Suppl 7): 45-52. https://doi.org/10.1053/j.seminoncol.2004.03.045
She, J., Yang, P., Hong, Q. and Bai, C., 2013. Lung cancer in China: Challenges and interventions. Chest, 143: 1117-1126. https://doi.org/10.1378/chest.11-2948
Sohal, S.S., Reid, D., Soltani, A., Ward, C., Weston, S., Muller, H.K., Wood-Baker, R. and Walters, E.H., 2010. Reticular basement membrane fragmentation and potential epithelial mesenchymal transition is exaggerated in the airways of smokers with chronic obstructive pulmonary disease. Respirology, 15: 930-938. https://doi.org/10.1111/j.1440-1843.2010.01808.x
Song, J., Shu, L., Zhang, Z., Tan, X., Sun, E., Jin, X., Chen, Y. and Jia, X., 2012. Reactive oxygen species-mediated mitochondrial pathway is involved in Baohuoside I-induced apoptosis in human non-small cell lung cancer. Chem. Biol. Interact., 199: 9-17. https://doi.org/10.1016/j.cbi.2012.05.005
Vu, T., Jin, L. and Datta, P.K., 2016. Effect of cigarette smoking on epithelial to mesenchymal transition (EMT) in lung cancer. J. clin. Med., 5: 44. https://doi.org/10.3390/jcm5040044
Wang, Y.C., Sung, W.W., Wu, T.C., Wang, L., Chien, W.P., Cheng, Y.W., Chen, C.Y., Shieh, S.H. and Lee, H., 2012. Interleukin-10 haplotype may predict survival and relapse in resected non-small cell lung cancer. PLoS One, 7: e39525. https://doi.org/10.1371/journal.pone.0039525
Wang, Y., Zhai, W., Wang, H., Xia, X. and Zhang, C., 2015. Benzo(a)pyrene promotes A549 cell migration and invasion through up-regulating Twist. Arch. Toxicol., 89: 451-458. https://doi.org/10.1007/s00204-014-1269-8
Yue, P. and Turkson, J., 2009. Targeting STAT3 in cancer: How successful are we? Exp. Opin. Investig. Drugs, 18: 45-56. https://doi.org/10.1517/13543780802565791
To share on other social networks, click on any share button. What are these?










