The Effect of Visual Input on Postural Stability in Healthy Subject Based on New Method of Measurement
Research Article
The Effect of Visual Input on Postural Stability in Healthy Subject Based on New Method of Measurement
Monireh Ahmadi Bani1*, Mostafa Kamali2, Iman Borji3, Soheyla Aslani3, Francis Fatoye4
Abstract | Clinically, the Romberg test has been used for evaluating stability in patients with various neurological defects. This test evaluates patients in 1 minute standing, but studies have shown that any stability test performed for less than five minutes is not clinically valuable. This study has evaluated stability with open and close eyes in normal subjects during five minutes standing in twenty healthy subjects. The subjects were asked to stand on a force plate for one and then five minutes, respectively. Their stability parameters were evaluated based on the old and new methods. Paired sample t-test was used for comparison between two methods and different conditions (eyes open and eyes closed). Traditional method for stability analysis showed no difference between two conditions in one minute standing (p ≥ 0.05). However, the new method confirmed that stability parameters significantly decreased in five minutes standing (p < 0.001). Moreover, patients were unstable in standing during the fourth and fifth minute. Taken together, diagnosis based on five minute standing using the Romberg test appear to be sensitive and accurate than one minute.
Editor | Arezoo Eshraghi, PhD in Orthotics and Prosthetics, Bloorview Research Institute, Holland Bloorview Kids Rehabilitation Hospital, Toronto, Canada.
Received | October 15, 2015; Revised | December 22, 2015; Accepted | December 25, 2015; Published | Febuary 14, 2016
*Correspondence | Monireh Ahmadi Bani, University of Social Welfare and Rehabilitation Science, Kodakyar Street, Daneshjo Boulevard, Evin, Tehran, Iran, E-mail: M.ahmadi_bani@yahoo.com
Citation | Bani, M. A., M. Kamali, I. Borji, S. Aslani and F. Fatoye (2016). The effect of visual input on postural stability in healthy subject based on new method of measurement. Health Rehabil. 1(1): 5-10.
Keywords | Standing stability, Prolonged standing, Force plate
Introduction
Ability to stand and walk independently is based on the performance of neuromuscular system. Moreover, three important systems contributing to postural control include the visual, vestibular, and somatosensory systems (Collins and De Luca, 1995; Nashner et al., 1982; Hu and Woollacott, 1994). Vestibular inputs were produced by linear and angular accelerations of the head. Somatosensory inputs (e.g. proprioceptive and cutaneous sensation) are being simulated by contact forces and motions of the extremities. Visual inputs are resultant of linear and angular motions of the visual field. The role of each of these physiological systems (vision, somatosensory and vestibular inputs) is examined by removing one of these modalities in laboratory settings and then the subject’s postural control is evaluated.
The most popular protocol for assessing visual contribution in maintenance of balance is Romberg test (Black et al., 1982; Dichgans et al., 1976; Paulus et al., 1984: Paulus et al., 1989; Ring et al., 1989). In this test, subjects are examined in quiet standing in two conditions include open and close eyes and postural sway is calculated by a force platform. Various parameters used to measure stability including excursion of centre of pressure (COP), velocity of COP sways and path length sways in Anterior-Posterior (A-P) and Medial-Lateral (M-L) planes.
Clinically, the Romberg test has been used for evaluating stability in patients with various neurological defects such as spinal cord injury (SCI) and multiple sclerosis (MS) (Njiokiktjien and De Rijke, 1972; Collins and De Luca, 1995). Removing one of these inputs (visual, vestibular, and somatosensory systems) decreases standing stability significantly (1, 6). From a motor control viewpoint, postural sway increases when a subject closes his or her eyes (Collins and De Luca, 1995; Paulus et al., 1984) and this is an indication of instability. Standing stability has being evaluated using force plate based on Romberg test (the duration of the test is one minute) (Khasnis and Gokula, 2003).
However, it has been shown that sensitivity and accuracy of stability analysis in five minutes is a more effective approach than traditional method (one minute stability test) to analysis standing stability of patients (Tagi Karimi et al., 2014; Karimi and Esrafilian, 2013). Duarte and Zatsiorsky showed that after 5 minutes COP shift in A-P about 17 millimeters and after 3 minutes and 30 seconds shift M-L about 22 millimeters (Duarte and Zatsiorsky, 1999). Although Karimi and Esrafilian in their study demonstrated that foundation on the traditional method (1 minute standing), the SCI and Perthes patients were more stable than normal subjects but based on the new method (5 minute standing) these groups were unstable than normal adults (Karimi and Esrafilian, 2013). In other studies, significant differences between stability parameters in the first and fifth minutes (Tagi Karimi et al., 2014; Taghi Karimi et al., 2013). It has been demonstrated that the unstable position occurred in the third and fifth minutes (Esrafilian et al., 2013; Karimi and Esrafilian, 2013).
Romberg test (as a standard test) by open and close eyes has been used for assessing stability in less than 1 minute but recent studies reported instability is demonstrated in third and fifth minute. Since there is no study evaluating the influence of vision in prolonged standing, the aim of this study was to evaluate the stability with open and close eyes in normal subjects during prolonged standing. This study will contribute the effect of vision input in stability and balance in prolonged standing.
Method
Subjects
Twenty healthy adult subjects participated in the study. Table 1 shows the characteristics of the subjects participated in this study. Exclusion criteria included any known history of musculoskeletal or neurologic disorders or any other medical condition that would affect their stability such as visual or hearing impairments. Ethical approval was obtained from Isfahan University of Medical Sciences, Ethical Committee. Informed written consent was obtained from each subject before data collection.
Table 1: The characteristics of the subjects participated in this research project
|
Participants |
Number |
Age |
Mass |
Height |
|
Healthy subjects |
20 |
22±5 |
63±7.5 |
1.65±0.12 |
Equipment
A Kistler force platform with piezoelectric force transducer was used to measure ground reaction forces (GRF) from which COP data were calculated in horizontal plane. Data were collected at 100 Hz for conditions of quiet one and five minutes standing. Stability was evaluated by calculating some parameters such as COP excursions in mediolateral and anteroposterior directions, velocity of COP sways in mediolateral and anteroposterior directions, and path length of COP in these planes based on the following equations:
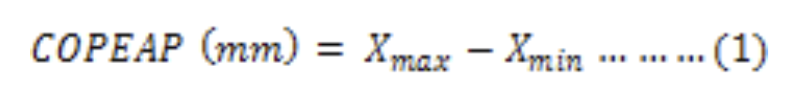
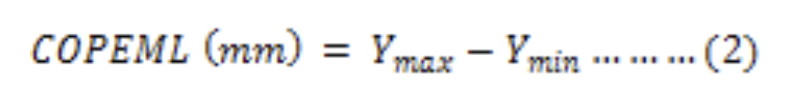
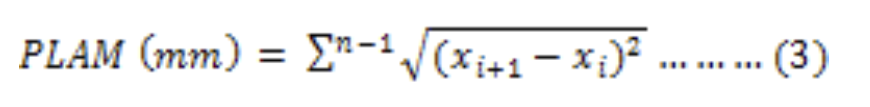
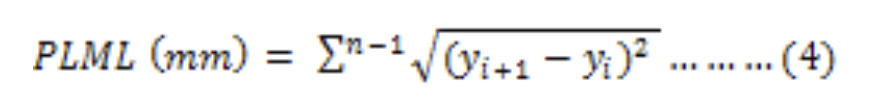
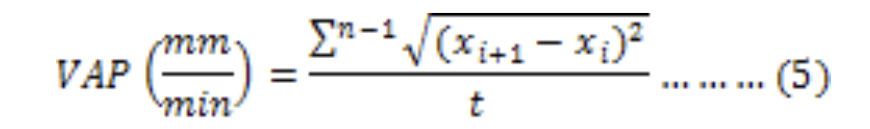
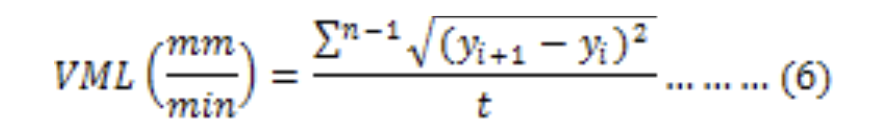
Where, COPEAP, COPEML, PLAP, PLML, VAP, and VML are the excursion of the center of pres sure in the anteroposterior direction, excursion of the center of pressure in the mediolateral direction, path length in the anteroposterior direction, path length in the mediolateral direction, velocity of the COP in the
Table 2: COP in A-P and M-L direction with and without input
|
Mean COP excursion in anteroposterior plane (closed eyes) |
29.2± 23 |
27.9± 17 |
29.4± 18 |
27.1± 17 |
31.2± 22 |
26.5± 15 |
28.4± 19 |
29.5± 17 |
27.3± 18 |
27.7± 19 |
25.4± 14 |
28.0± 14 |
26.5 ± 14 |
29.7± 18 |
|
Mean COP excursion in anteroposterior plane (opened eyes) |
30.2 ± 28 |
32.8 ± 31 |
25.9 ± 11 |
26.1 ± 17 |
24.6 ± 12 |
25.4 ± 14 |
25.7 ± 16 |
22.2 ± 9 |
26.1 ± 19 |
27.6 ± 19 |
24.2 ± 13 |
27.7 ± 15 |
30.4 ± 22 |
28.0 ± 17 |
|
Mean COP excursion in mediolateral plane (closed eyes) |
14.1± 7 |
15.8± 7 |
18.7± 13 |
15.1 ± 10 |
15.8 ± 10 |
19.6 ± 17 |
18.7 ± 16 |
17.4 ± 10 |
17.6 ± 12 |
19.0 ± 27 |
20.5 ± 27 |
15.8 ± 10 |
15.0 ± 9 |
18.2 ± 12 |
|
Mean COP excursion in mediolateral plane (opened eyes) |
13.9 ± 7 |
16.4 ± 6 |
17.0 ± 12 |
13.2 ± 10 |
14.4 ± 9 |
13.3 ± 17 |
13.1 ± 15 |
14.1 ± 10 |
16.0 ± 12 |
17.5 ± 27 |
16.7 ± 27 |
17.0 ± 10 |
17.0 ± 9 |
17.1 ± 12 |
Table 3: Path of length COP in A-P and M-L direction with and witjout vision input
|
Path length of COP in anteroposterior direction (closed eyes) |
484.1 ± 219 |
451.4 ± 195 |
481.8 ± 208 |
452.9 ± 178 |
451.2 ± 196 |
467.8 ± 202 |
469.8 ± 177 |
443.1 ± 158 |
467.9 ± 178 |
448.7 ± 166 |
468.5 ± 178 |
459.6 ± 179 |
441.2 ± 172 |
453.4 ± 170 |
|
Path length of COP in anteroposterior direction (opened eyes) |
435.1 ± 172 |
422.5 ± 111 |
410.8 ± 71 |
399.2 ± 107 |
396.1 ± 78 |
402.8 ± 93 |
425.6 ± 142 |
409.7 ± 129 |
402.4 ± 105 |
401.7 ± 88 |
408.2 ± 89 |
400.2 ± 96 |
408.6 ± 98 |
412.8 ± 95 |
|
Path length of COP in mediolateral direction (closed eyes) |
582.0 ± 354 |
562.1 ± 363 |
612.6 ± 394 |
558.2 ± 346 |
568.8 ± 401 |
586.6 ± 430 |
595.1 ± 355 |
541.0 ± 312 |
591.8 ± 362 |
561.0 ± 367 |
597.5 ± 369 |
580.9 ± 353 |
553.3 ± 355 |
553.3 ± 344 |
|
Path length of COP in mediolateral direction (opened eyes) |
485.4 ± 355 |
488.3 ± 363 |
491.0 ± 392 |
465.5 ± 347 |
475.8 ± 400 |
478.6 ± 430 |
500.1 ± 356 |
495.6 ± 311 |
480.9 ± 362 |
481.3 ± 368 |
496.2 ± 366 |
478.6 ± 354 |
474.6 ± 356 |
492.2 ± 345 |
anteroposterior direction, and velocity of the COP in the mediolateral direction, respectively (12).
Procedure
Prior data collection, the subjects were allowed to get a balanced standing position on the force platform. Then they were asked to stand quietly on the force plate for five minutes in anatomical comfortable position (looking straight ahead with their head erect and their arm at their sides). Subjects were instructed not to touch their lower extremities with their hands to prevent stabilization of extended physiologic proprioception caused by fingers sensory feedback and they analyzed with open and close eyes by random.
Randomization minimizes risk of possible fatigue as a confounding variable. Butterworth low pass filter with 10 Hz frequency was used to minimize errors in sway path calculation due to high frequency noise. Data were divided each 20 second periods (Karimi and Esrafilian, 2013). The first 20 seconds of the data were eliminated to avoid the effect of undesirable initial movement of standing. Subjects were also asked to stand on the force plate for a minute (based on traditional method). The second third of the data (between 20 and 40 seconds) were used for final analysis.
Statistical analysis
Shapiro-Wilk test revealed that the data was normally distributed. The minimum value of COP, velocity and sum of path were selected as most stable frame. Other frame was evaluated by paired T-test with significance level set at p=0.05. The frame is near to unstable if difference was significant by considering alpha 0.05 that is shown by red colour and is unstable by considering alpha 0.05 that is shown by dark red. The frame is stable if it was not significant. Differences between eyes open and eyes close based on new (regardless of frame time) and traditional method was evaluated using paired T test. The differences between stability parameters under the two test conditions for traditional based test were evaluated by paired t test.
Results
The mean and standard deviation values of stability parameters for these conditions (eyes open and eyes closed) are shown in Tables 2 to 4. Tables 2, 3 and 4 display variations between mean values of stability parameters in different frames time. Stability pattern in five minute quiet standing is shown by dark and light green color representative unstable and stable position, respectively.
There are significant differences in COP M-L (p = 0.01), and A-P, M-L and M-L and A-P direction (both p < 0.001) in eyes closed and eyes open conditions. However, there was no significant difference in COP A-P (p = 0.195). Table 4 shows the mean and values of stability parameters under both conditions (eyes closed and eyes open).
Stability of the subjects was also evaluated based on the traditional method. The mean values of COP excursions in the mediolateral and anteroposterior directions were 32.86±31.7mm and 16.43±9.3 mm during opened eyes, respectively compare to 27.98±17.3 and 15.44±7.56 mm during closed eyes
Table 4: Velocity in A-P and M-L direction with and without vision input
|
Velocity of COP in anteroposterior direction (closed eyes) |
968.3 ± 438 |
902.9 ± 390 |
963.7 ± 416 |
905.8 ± 356 |
902.4 ± 392 |
935.6 ± 404 |
939.7 ± 355 |
886.3 ± 316 |
935.8 ± 356 |
897.5 ± 333 |
937.0 ± 357 |
919.3 ± 359 |
882.4 ± 344 |
906.8 ± 340 |
|
Velocity of COP in anteroposterior direction (opened eyes) |
870.2 ± 444 |
845.0 ± 400 |
821.6 ± 427 |
798.4 ± 373 |
792.3 ± 404 |
805.7 ± 416 |
851.2 ± 369 |
819.4 ± 325 |
804.8 ± 371 |
803.5 ± 353 |
816.4 ± 370 |
800.4 ± 376 |
817.3 ± 361 |
825.6 ± 358 |
|
Velocity of COP in mediolateral direction (closed eyes) |
1164.1 ± 708 |
1124.3 ± 726 |
1225.3 ± 788 |
1116.5 ± 693 |
1137.7 ± 803 |
1173.3 ± 861 |
1190.2 ± 710 |
1082.0 ± 624 |
1183.6 ± 725 |
1122.0 ± 734 |
1195.0 ± 738 |
1161.9 ± 707 |
1106.6 ± 710 |
1106.7 ± 688 |
|
Velocity of COP in mediolateral direction (opened eyes) |
971.6 ± 242 |
970.6 ± 223 |
977.9 ± 195 |
925.5 ± 232 |
939.2 ± 201 |
952.5 ± 230 |
1005.3 ± 378 |
980.2 ± 347 |
948.7 ± 227 |
951.2 ± 204 |
983.5 ± 232 |
956.9 ± 231 |
949.4 ± 219 |
990.8 ± 225 |
Table 5: Comparison stability parameters between open and close eyes with new and traditional method
|
Conditions |
COPX |
COPY |
Velocity X |
Velocity Y |
Path length X |
Path length Y |
|
Opened Eyes based on traditional method |
32.86 ± 31.7 |
16.43 ± 9.3 |
422.5 ± 111.5 |
488.4 ± 112.6 |
854 ± 223 |
970.7 ± 223 |
|
Closed Eyes based on traditional method |
27.98 ± 17.3 |
15.44 ± 7.56 |
451.4 ± 195.3 |
562.1 ± 363 |
902.96 ± 390.7 |
1124 ± 726 |
|
P-value |
0.157 |
0.34 |
0.27 |
0.198 |
0.27 |
0.189 |
|
Opened Eyes based on new method |
26.96 ± 18.6 |
15.52 ± 11.13 |
819.46 ± 213.77 |
964.577± 242.91 |
409.73 ± 106.88 |
484.63 ± 122.531 |
|
Closed Eyes based on new method |
28.17 ± 17.81 |
17.25 ± 14.98 |
920.31 ± 362.56 |
1149.27 ± 716.04 |
460.15 ± 181.28 |
574.63 ±358.022 |
|
P-value |
0.195 |
0.000 |
0.000 |
0.000 |
0.000 |
0.000 |
(p=0.15 and 0.34, respectively). The velocities of COP sways in anteroposterior direction were 422.5 ± 111.5 mm/min and 451.4 ± 195.3 mm/min during eyes open and eyes closed, respectively (p=0.27). Table 5 shows the mean values of stability parameters under both opened and closed eyes conditions, based on the traditional approach. As it can be seen from the table there were no differences between the test conditions.
Discussion
This study investigated the effects of time of standing with open and close eyes on the stability parameters during five minute standing to evaluate the hypothesis that Romberg test in five minute is more accurate than just 1 minute. Most patients with neurological and musculoskeletal disorders with balance impairment show stable posture in 1 minute while they cannot control their stability in five minute (11, 12). However, the most of activity daily living such as talking, washing the dishes, waiting for a taxi or standing in a work environment need prolonged period of standing.
Long quiet standing for five minutes was chosen for this study not only to mimic real daily living situation but also to challenge stability in different temporal frame to magnify balance proceeding in normal healthy subjects. Although muscle fatigue is a normal response to prolonged standing but an early, excessive and chronic fatigue is abnormal and is indicator of a neuromuscular disorder (Neumann, 2002).
A previous study in this field showed three COP relocation pattern during long standing (Duarte and Zatsiorsky, 1999). Movement in body segment specially arm, head and trunk, also weight transfer from one leg to another result decrease influence of fatigue and control of stability cause COP movement. But the important matter is the ability of subjects to move from unstable position to stable position (Karimi and Esrafilian). Another study confirmed that using one-minute stability test did not show instability in patients with musculoskeletal disorders (Karimi and Esrafilian., (2013)). Tagi Karimi et al. (2014) reported a theory, during 1 minute standing children with Perthes and subjects with spinal cord injury were more stable than healthy subjects, while in five minutes standing there is not accurate. That study also reported that the most unstable position was in third and fifth minutes (Karimi and Esrafilian). The present study also showed that the most stable position was in the second and most unstable position was in the fourth and fifth minutes. These results are in accordance with Duarte and Zatsiorskysudy (Duarte and Zatsiorsky, 1999) and support karimi and Esrafilian theory (Karimi and Esrafilian, 2013)). These researchers demonstrated that five minutes stability test is more accurate for balance evaluation in patients with musculoskeletal disorders. Prolonged standing in five minute describes balance details.
The present study also showed that visual inputs play an important role within equilibrium control especially in sum of path and velocity. This study demonstrated that there were significant differences between in all of stability parameters under the eyes open and eyes closed, conditions except for the COP in anteroposterior direction. There are different mechanisms for control of postural stability in M-L and A-P direction. Hip motion strategy by activation in adductor and abductor muscles control M-L stability while ankle motion strategy by dorsiflexor and plantarflexor muscles control A-P stability (Winter et al., 1993). Weight transfer from one leg to another migrate COP more distances during eyes closed than eyes open. This result is shown by evaluation of progressing the data. Decreased postural stability was observed in subjects with vision loss compared with their healthy counterparts (Ray et al., 2008), while this instability is not shown in first 1 minute in most of patients. Traditional method shows no significant differences during eyes open and eyes closed while standing in five minutes confirms a decrease in stability, which may be due to visual input. Prolonged standing test demonstrates instability in these situations.
The present study highlights areas for future clinical research to better understand standing postural control and stability for persons with musculoskeletal and neurological disorders with stability problem. This study was done only in one trial with limited sample size. A study with a larger sample size may help to understand in more details the different frame times without evaluating repeatability of parameters. Comparison stability parameters between normal and amputee subject or people with different disorder is recommended in following studies for evaluation of stability.
CONCLUSIONS
The present study showed the most unstable time in five minute standing is fourth and fifth, that is better test for description instability details. Romberg test in five minutes is more accurate and sensitive than just 1 minute standing test because close eyes causes instability in minute fifth standing.
Conflict of interest
The authors report no conflicts of interest.
References
- Black FO, Wall III C, Rockette Jr HE Kitch R (1982). Normal subject postural sway during the Romberg test. Am. J. Otolaryngol. 3: 309-318. http://dx.doi.org/10.1016/S0196-0709(82)80002-1
- Collins J, De Luca C (1995). The effects of visual input on open-loop and closed-loop postural control mechanisms. Experimental brain research, 103, 151-163. http://dx.doi.org/10.1007/BF00241972
- Dichgans J, Mauritz K, Allum J, Brandt T (1976). Postural sway in normals and atactic patients: Analysis of the stabilising and destabilizing effects of vision. Agressologie: revue internationale de physio-biologie et de pharmacologie appliquees aux effets de l’agression, 17, 15.
- Duarte M, Zatsiorsky VM (1999). Patterns of center of pressure migration during prolonged unconstrained standing. Motor control. 3: 12-27.
- Taghi Karimi M, Jamshidi N, Bahreinizad H, Bani MS and Omar AH (2014). A new approach to measure stability during quiet standing. Work. 49: 663-8.
- Hu M-H, Woollacott MH (1994). Multisensory training of standing balance in older adults: I. Postural stability and one-leg stance balance. J. Gerontol. 49: M52-M61.
- Karimi M, Esrafilian A (2013). Evaluation of the stability of normal subjects and patients with Perthes and spinal cord injury disorders during short and long periods of time. Prosthetics and Orthotics International. 37: 22-29.
- Khasnis A, Gokula R (2003). Romberg’s test. Journal Of Postgraduate Medicine. 49: 169.
- Nashner LM, Black FO, Wall C (1982). Adaptation to altered support and visual conditions during stance: Patients with vestibular deficits. J. Neurosci. 2: 536-544.
- Neumann DA (2002). Kinesiology of the musculoskeletal system, Mosby/Elsevier.
- Njiokiktjien C, De Rijke W (1972). The recording of Romberg’test and its application in neurology. Agressologie: revue internationale de physio-biologie et de pharmacologie appliquأ©es aux effets de l’agression, 13, Suppl C: 1.
- Paulus W, Straube A, Brandt T (1984). Visual stabilization of posture physiological stimulus characteristics and clinical aspects. Brain. 107: 1143-1163. http://dx.doi.org/10.1093/brain/107.4.1143
- Paulus W, Straube A, Krafczyk S, Brandt T (1989). Differential effects of retinal target displacement, changing size and changing disparity in the control of anterior/posterior and lateral body sway. Exp. Brain Res. 78: 243-252. http://dx.doi.org/10.1007/BF00228896
- Ray CT, Horvat M, Croce R, Christopher Mason R, Wolf SL (2008). The impact of vision loss on postural stability and balance strategies in individuals with profound vision loss. Gait posture. 28: 58-61. http://dx.doi.org/10.1016/j.gaitpost.2007.09.010
- Ring C, Nayak U, Isaacs B (1989). The effect of visual deprivation and proprioceptive change on postural sway in healthy adults. Journal of the American Geriatrics Society. 37: 745. http://dx.doi.org/10.1111/j.1532-5415.1989.tb02237.x
- Taghi Karimi M, Jamshidi N, Bahreinizad H, Bani MS, Omar AH (2013). A new approach to measure stability during quiet standing. Work. 4.
- Winter D, Prince F, Stergiou P, Powell C (1993). Medial-lateral and anterior-posterior motor-responses associated with center of pressure changes in quiet standing. Neurosci. Res. Com. 12: 141-148.
To share on other social networks, click on any share button. What are these?



