Radiological Evaluation Of Acellular Fish Swim Bladder and Autologous Bone Marrow Clot on Induced Radial Bone Defects in Rabbits
Radiological Evaluation Of Acellular Fish Swim Bladder and Autologous Bone Marrow Clot on Induced Radial Bone Defects in Rabbits
Noorulhuda A. Mahdi, Nadia H.R. AL-Falahi*
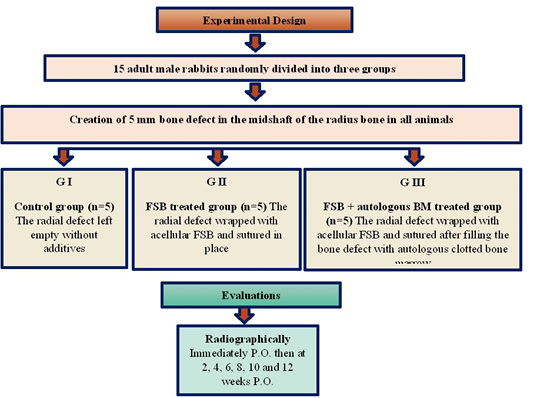
Experimental design.
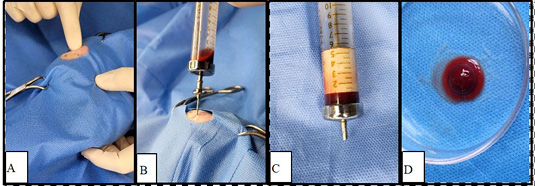
Steps of bone marrow aspiration; A: Palpating the greater trochanter; B: The aspiration needle is inserted toward the trochanteric fossa; C: The aspirated BM is left to clot before implantation; D: Bone marrow clot sample.
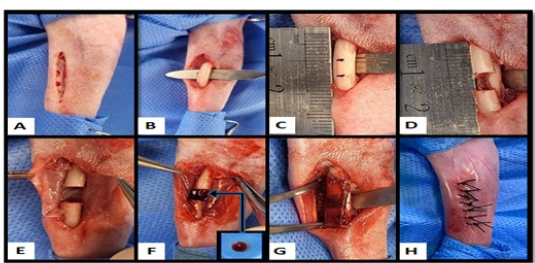
Steps of surgical procedure; A: 3–4 cm skin incision is performed on the right forelimb’s cranio-medial aspect; B: Expose the radius bone after separating the muscles; C: 5mm distance at the radius mid shaft is marked for osteotomy; D: Creation of 5mm segmental bone defect; E: The radial defect is wrapped with acellular FSB; F: The radial defect is filled with bone marrow clot after wrapping with acellular FSB; G: The FSB membrane is sutured; H: Sutured skin.
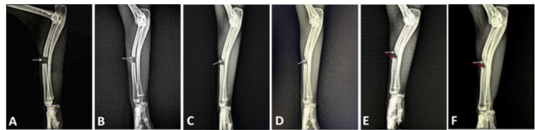
A mediolateral view of radiological image in control group (A) Immediately post –operation, shows a radiolucent segmental defect area appeared at the mid shaft of radius bone. (B) At 2nd week post –operation, shows the proximal and distal ends of the radius bone segments with a mild periosteal reaction. (C) At 4th week post –operation, shows thickening of both ends of the defect with callus formation directed from the proximal end of the radius defect towards the defect center and attached with the ulna. (D) At 6th week post –operation, callus formation was increased from the proximal end of the radius defect sloped to the center of the defect and fused with ulna. (E) At 8th week post –operation, mild periosteal reaction in the radius defect’s distal end. (F) At 12th week post –operation, the sloping callus from the radius defect’s proximal end to its center was continuously growing with radio-ulnar synostosis.
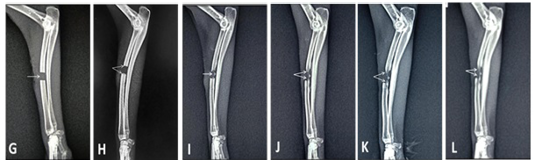
A mediolateral view of radiological image in FSB treated group. (G) Immediately post –operation, shows a radiolucent segmental defect area in the mid shaft of radius bone. (H) At 2nd week post –operation, shows a little periosteal response at both ends of the radius bone defect. (I) At 4th week post –operation, there was an increase in the periosteal reaction, and a radiopaque foci of newly formed bone is visible in the defect’s center. (J) At 6th week post –operation, the radius defect’s new bone growth was increased and extended from both ends. (K) At 8th week post –operation. there was an increase in newly formed bone and extended from both ends of the radius defect towards the central new bone formation foci. (L) At 12th week post –operation, shows increased the opacity of new bone formation and extended in a straight direction from both ends of the radius defect towards the central new bone formation foci, with partially bridging the radius defect.
A mediolateral view of radiological image in FSB-BMC treated group. (M) Immediately post –operation, shows a radiolucent segmental defect area in mid shaft of radius bone (N) At 2nd week post –operation, shows a slight periosteal reaction at both ends of the segmental radius defect with slight radiopaque foci in the center of the defect (O) At 4th week post –operation, shows increased the periosteal reaction at both ends of the segmental radius defect with increased the opacity of the foci in the center of the defect (P) At 6th week post –operation, shows increased new bone growth and it extended in a straight direction from the proximal to the distal end of the bone defect. (Q) At 8th week post –operation, the segmental bone defect had been bridged by an increase in callus formation opacity. (R) At 12th week post –operation, shows a complete bridging of the segmental defect of radius bone by new bone formation.