A Case of Recurrence of Hydatid Cyst in the Liver
Case Report
A Case of Recurrence of Hydatid Cyst in the Liver
Laveena Shekhawat, Sheethal S*
Geetanjali Medical College and Hospital, India.
Abstract | Introduction: Hydatid cyst is a parasitic infection caused by Echinococcus granulosus commonly termed as dog tapeworm. However, man is an accidental host and develops symptoms of the disease in organs where the eggs get lodged, the most common being the liver. Case report: A 29-year-old male presented with pain in the right upper quadrant with radiation towards the back along with abdominal fullness for 5-7 days. Physical examination and imaging investigations were performed on the patient which revealed the diagnosis. Results: The patient underwent laparoscopic deroofing procedure and the cyst was sent to pathology and microbiology sections for laboratory diagnosis. Identification of sickle shaped hooklets on wet mount and ZN staining confirmed the diagnosis. The patient received post-operative oral albendazole which he failed to start immediately leading to recurrence of the parasitic hepatic cyst. Conclusion: Treatment is a combination of surgery and post-op anti-parasitic drugs. Delay in initiating albendazole therapy can lead to recurrence of the cysts in the same sites.
Keywords | Cystic ecchinococcosis, Ecchinococcus granulosus, Hepatic cyst, Parasitic cyst of liver, Liver parasite
Editor | Muhammad Imran Rashid, Department of Parasitology, University of Veterinary and Animal Sciences, Lahore, Pakistan.
Received | July 04, 2022; Accepted | August 22, 2022; Published | December 15, 2022
*Correspondence | Sheethal, Geetanjali Medical College and Hospital, India; Email: dr.sheethal_s@yahoo.com
Citation | Shekhawat L, Sheethal S (2022). A Case Of Recurrence Of Hydatid Cyst In The Liver. J. Adv. Parasitol. 9(1): 37-40.
DOI | http://dx.doi.org/10.17582/journal.jap/2022/9.1.37.40
ISSN | 2311-4096

Copyright: 2022 by the authors. Licensee ResearchersLinks Ltd, England, UK.
This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
INTRODUCTION
Cystic echinococcosis (CE) is a parasitic illness caused by infection with dog tapeworms (Echinococcus granulosus and Echinococcus multilocularis) in their larval stage (Li et al, 2016). The global prevalence of CE is estimated at 2 to 3 million human cases with an estimated mortality rate of 2 to 4% per 100 inhabitants (Manzano-Román et al., 2015). It has been included in the list of neglected tropical diseases and is considered to be one of the six priority neglected zoonotic diseases (Malla and Mewara, 2016).
Although CE is endemic in many regions of India, the detailed epidemiological studies from India are scanty (Malla and Mewara, 2016). This parasite exhibits a predilection for the liver (70-80%) followed by the lungs (20-30%) with involvement of spleen, kidney, heart, brain, bone and breasts being less common (Wuestenberg et al., 2014). The definitive host for the parasite is dogs, whereas animals such as sheep, cattle, goats and camels serve as intermediate hosts (Mandal and Mandal, 2012). Humans are dead end, occasional, intermediate hosts and acquire the infection through accidental ingestion of echinococcus eggs excreted in dog feces and transmitted through a close contact with infected animals (Picolli et al., 2014).
The size, number of cysts and type of infecting parasite will decide the clinical manifestations of the hydatid disease. Common symptoms include fever, chills, nausea, dyspnea, dysphagia and pain in the right upper quadrant. Rupture of a large echinococcal cyst causes severe anaphylactic reaction, however smaller cysts remain asymptomatic and get lodged in distant organs. Diagnosis of hydatid cyst can be made on the basis of history of exposure, serological tests, and radiological images. Radiological findings differ depending on the stage of the cyst (Pakala et al., 2016).
Radical surgery remains the main stay of therapy as conservative surgical procedure usually ends up in risking the patient’s life by developing anaphylactic reactions. However, surgery combined with chemotherapy started before surgery and continued up to 8 weeks post-op has been found to be the most successful existing therapy (Anand et al., 2012).
CASE PRESENTATION
A 29-year-old apparently healthy man started experiencing pain in the right upper quadrant radiating to the back associated with abdominal fullness for 5-7 days. There was no significant occupational history and the patient had no contact with dogs either. However, the patient gave a dietary history of being a non-vegetarian. There was no other significant past history.
On physical examination, the patient was afebrile with no signs of pallor, icterus, cyanosis, edema or lymphadenopathy. His pulse was 79 bpm (beats per minute) with a regular BP (blood pressure) of 120/80 mm of Hg. On per abdominal examination, a mass was palpated in the right lobe of liver. The patient was advised computed tomography (CT) scan of the liver.
Routine investigations showed a total leucocyte count of 12.9 per µl3 and a hemoglobin level of 16 mg/ml. Contrast-enhanced dynamic CT scan of the upper abdomen revealed that the liver was enlarged with evidence of 10.4 cm × 7.7 cm × 7.4 cm sized thin-walled hypodense cystic lesion in the 7th segment. Multiple enlarged mesenteric and paraaortic lymph nodes were noted.
The patient underwent surgery. The procedure performed was cyst removal by laparoscopic deroofing and omentoplasty. The contents were sent to the Department of Pathology for histopathological examination and to the Department of Microbiology for microscopy of cystic fluid.
The specimen received in the Department of Pathology consisted of multiple fragmented cysts.
Gross examination: A partially embedded cyst with a rough external surface and a glistening internal surface, totally measuring 7 cm × 5 cm × 1.5 cm in dimensions (Figure 1).
The following examinations were performed with the fluid received in the Department of Microbiology:
Wet mount examination showed colorless sickle shaped hooklets measuring 20-40 µm in size morphologically resembling Echinococcus spp. (Figure 2).
Modified Ziehl-Neelsen staining showed pink colored acid fast hooklets. (Figure 3).
The patient was prescribed oral albendazole for a month post-op and discharged. When the patient visited the OPD for follow-up after 15 days, USG abdomen was performed which revealed formation of new cysts in the operated site. On enquiring, the patient revealed that he did not start the anti-parasitic agent until 10 days post-op. Now, the patient is being monitored by repeated follow-ups to assess the growth and development of the cyst.
DISCUSSION
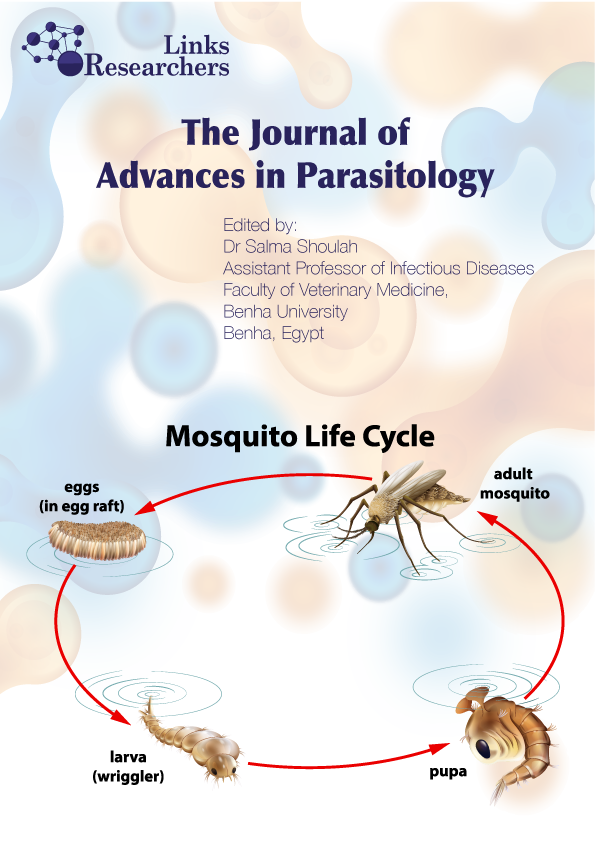
The life cycle of the parasite Ecchinococcus granulosus has three separate developmental stages: adult worms in the intestines of the definitive host, its eggs in the environment and the metacestode (hydatid cyst) in the intermediate host (Manzano-Román et al., 2015; Mandal and Mandal, 2012). Carnivores, especially dogs, are the definitive hosts and common intermediate hosts are sheep, goats, cattle, camels and pigs. Human act as accidental intermediate hosts. They acquire the infection by ingestion of eggs in the contaminated food (Wuestenberg, 2014). In the small intestine, eggs hatch into oncospheres which penetrate the intestinal wall and via the bloodstream enter into the internal organs of the body (Mandal and Mandal, 2012).
Most of the time, hydatid disease is asymptomatic for a long period of time as the cysts grow very slowly. Cysts may be solitary or multiple and present as a vague abdominal mass and pain due to pressure effects on adjacent organs / structures (Pakala et al., 2016). Right upper abdominal or epigastric pain or fullness associated with a palpable mass are common symptoms of hepatic hydatid cyst (Safioleas et al., 2006; Kumar et al., 2003).
Non-specific tests such as serum bilirubin, serum alkaline phosphatase, total leucocyte count, eosinophil count may be inconclusive, non-invasive confirmation of the diagnosis can usually be accomplished by combined use of radiologic imaging and immunodiagnostic techniques. Clinical diagnostic methods like ultrasonography (USG) not only helps in diagnosis, but also in treatment and follow up of the patients. Computed tomography (CT) scan is preferred in cases where USG fails due to patient related difficulties such as obesity or any history of previous surgeries (Anand et al., 2012). Nowadays, serological tests are gaining popularity to confirm a suspected radiologic diagnosis. Enzyme linked immunosorbent assay (ELISA), indirect hemagglutination (IHA) tests, immunoelectrophoresis and immunoblot tested with in-house prepared antigens from hydatid fluid are used are serological tests to diagnose CE (Manzano-Román et al., 2015; Ortona et al., 2000). Laboratory confirmation of hydatid cyst is by wet mount identification or identification on stained smears of the hydatid fluid. Scolices, protoscolices and hooklets can be demonstrated (Malla and Mewara, 2016).
Being one among the most neglected parasitic diseases, new treatment modalities and discovery of new anti-parasitic agents are lacking for CE (Picolli et al., 2014). Based on the WHO classification, the suggested main stay of treatment remains surgery which is either conservative or radical with adjunct albendazole therapy. However, 20% of cases report back with recurrence after surgery for liver hydatid cysts. Depending on how the cysts develop further and what complications it brings to the patient, recurrent cysts can be left alone with adequate follow-up or percutaneous surgical measures can be employed (Anand et al., 2012). A non-randomized clinical trial concluded that either liposomal or tablet formulations of albendazole can be used to treat both single cysts and multiple daughter cysts of hepatic hydatid disease (Li et al., 2016).
CONCLUSION
Echinococcosis is a challenging clinical problem throughout the world. Early diagnosis by imaging modalities is helpful in endemic countries. Simple wet mount examination of hydatid fluid in resource poor settings can confirm the diagnosis. Eradication of the parasite surgically is essential along with a prophylactic dosage of albendazole. Recurrence is commonly noted in up to 20% cases, especially in patients who have not received albendazole therapy promptly during and after surgery.
CONFLICT OF INTEREST
There are no conflicts of interest to report.
Novelty Statement
Our study highlights that the follow up of albendazole medication in patients who have undergone surgical removal of hydatid cyst especially in the liver is very essential to make sure that recurrence is prevented. The patient can be started on the antiparasitic drug before discharge from the hospital so that continuation at home can be ensured.
Authors Contribution
Laveena Shekhawat: Literature search, Data analysis, Manuscript preparation and Manuscript editing.
Sheethal S: Concepts, Design, Definition of intellectual content, Literature search, Data anaylysis, Manuscript preparation, Manuscript editing, Manuscript review and Guarantor.
REFERENCES
Kumar MJ, Toe K, Banerjee RD (2003). Hydatid cyst of liver. Postgrad Med. J. 79(928):113–114. https://doi.org/10.1136/pmj.79.928.113
Li H, Song T, Shao Y, Aili T, Ahan A, Wen H (2016). Comparative Evaluation of Liposomal Albendazole and Tablet-Albendazole Against Hepatic Cystic Echinococcosis: A Non-Randomized Clinical Trial. Medicine. 95(4):e2237. https://doi.org/10.1097/MD.0000000000002237
Mandal S, Mandal MD (2012). Human cystic echinococcosis: epidemiologic, zoonotic, clinical, diagnostic and therapeutic aspects. Asian Pac. J. Trop. Med. 5(4):253–260. https://doi.org/10.1016/S1995-7645(12)60035-2
Manzano-Román R, Sánchez-Ovejero C, Hernández-González A, Casulli A, Siles M (2015). Serological Diagnosis and Follow-Up of Human Cystic Echinococcosis: A New Hope for the Future? BioMed. Res. Int. 2015:1-9. https://doi.org/10.1155/2015/428205
Ortona E, Riganò R, Margutti P, Notargiacomo S, Ioppolo S, Vaccari S, Barca S, Buttari B, Profumo E, Teggi A, Siracusano A (2000). Native and recombinant antigens in the immunodiagnosis of human cystic echinococcosis. Parasit. Immunol. 22(11):553–559. https://doi.org/10.1046/j.1365-3024.2000.00336.x
Pakala T, Molina M, Wu GY (2016). Hepatic Echinococcal Cysts: A Review. J. Clin. Transl. Hepatol. 28;4(1):39–46. https://doi.org/10.14218/JCTH.2015.00036
Piccoli L, Tamarozzi F, Cattaneo F, Mariconti M, Filice C, Bruno A, Brunetti E (2014). Long-term Sonographic and Serological follow-up of Inactive Echinococcal Cysts of the Liver: Hints for a “Watch-and-Wait” approach. PLoS Negl. Trop. Dis. 8(8):e3057. https://doi.org/10.1371/journal.pntd.0003057
S Anand, S Rajagopalan, Mohan R (2012). Management of liver hydatid cysts – Current perspectives. Med. J. Armed Forces India. 68(3):304–309. https://doi.org/10.1016/j.mjafi.2012.04.010
Safioleas MC, Misiakos EP, Kouvaraki M, Stamatakos MK, Manti CP, Felekouras ES (2006). Hydatid Disease of the Liver: A Continuing Surgical Problem. Arch. Surg. 141(11):1101–1108. https://doi.org/10.1001/archsurg.141.11.1101
Wuestenberg J, Gruener B, Oeztuerk S, Mason RA, Haenle MM, Graeter T, Akinli AS, Kern P, Kratzer W (2014). Diagnostics in cystic echinococcosis: Serology versus ultrasonography. Turk. J. Gastroenterol. 25(4):398–404. https://doi.org/10.5152/tjg.2014.7112
To share on other social networks, click on any share button. What are these?