Journal of Animal Health and Production
Case Report
Diagnosis and Medical Management of Oesophageal Penetration in an Abused Dog
Delna Mazda1, Ikhwan Saufi Ahamad Azahari2, Muhammad Waseem Aslam1, Puteri Azaziah Megat Abdul Rani2, Seng Fong Lau1*
1Department of Veterinary Clinical Studies, Faculty of Veterinary Medicine, Universiti Putra Malaysia (UPM), 43400 UPM, Serdang, Selangor, Malaysia; 2Department of Companion Animal Medicine and Surgery, Faculty of Veterinary Medicine, Universiti Putra Malaysia (UPM), 43400 UPM, Serdang, Selangor, Malaysia.
Abstract | An adult male local breed dog was referred with the signs of haematemesis, haemoptysis and swelling at the ventral neck region. History revealed removal of a wooden stick from the oral cavity a day before presentation. Physical examination revealed a sublingual hematoma. Complete blood count revealed marked neutrophilic leucocytosis with left shift and low thrombocyte count. Serum biochemistry profile showed marked hyperglobulinaemia, elevated alanine aminotransferase and alkaline phosphatase. Radiographic examination revealed presence of a round soft tissue or fluid opacity structure just ventral to the larynx and multiple small rounded air opacities coalescing to linear gas opacities in bilateral fascial planes of the neck. Computed tomography (CT) scan revealed multiple small rounded air densities coalescing to form linear gas–attenuating density in the periphery of oesophagus, indicating cervical soft tissues emphysema. The dog was managed medically and regained appetite four days after hospitalisation. The dog was discharged after five days of hospitalization. No recurrence of clinical signs was reported.
Keywords | Oesophageal penetration, CT, emphysema, dog, Medical management
Received | July 15, 2020; Accepted | August 05, 2020; Published | February 20, 2021
*Correspondence | Seng Fong Lau, Department of Veterinary Clinical Studies, Faculty of Veterinary Medicine, Universiti Putra Malaysia (UPM), 43400 UPM, Serdang, Selangor, Malaysia; Email: [email protected]
Citation | Mazda D, Azahari ISA, Aslam MW, Rani PAMA, Lau SF (2021). Diagnosis and medical management of oesophageal penetration in an abused dog. J. Anim. Health Prod. 9(2): 132-135.
DOI | http://dx.doi.org/10.17582/journal.jahp/2021/9.2.132.135
ISSN | 2308-2801
Copyright © 2021 Lau et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
Oesophageal injuries commonly occur in dogs with a history of chewing or playing with wooden sticks (Doran et al., 2008). Clinical signs at presentation differ with the duration of the injury. In cases of acute injury (<7days), dogs are presented with dysphagia and hypersalivation often with a mixture of blood and oral pain. Cases left untreated may progress to depressed behavior, loss of appetite, swelling of the cervical region, dyspnea and even shock. While in chronic cases (>7days), abscessation and discharging sinuses are commonly seen (Griffiths et al., 2000). Diagnosis is commonly made based on the history; however, some cases show the presence of cervical emphysema on radiographs indicating perforation of the pharyngeal wall or oesophagus. The presence of gas can be observed as gas attenuating densities on the Computed Tomography (CT) Scan. (Lamb et al., 2016). Treatment varies amongst cases depending on the presenting signs. In cases with lodged wooden fragments, treatment of choice is per oral endoscopic removal of the fragment or advancement into the stomach (Teh et al., 2018). Smaller perforations however without presence of wooden fragments can be managed medically (Teh et al., 2018). The present report describes a case of oesophageal perforation in a dog that was diagnosed radiologically and invasiveness of the perforation was estimated by CT scan, and finally managed by medical intervention.
Case Signalment, History and Clinical Findings
An adult 16 Kg (35.3 lb), intact male mongrel dog was referred to the University Veterinary Hospital, Universiti Putra Malaysia (UVH–UPM) for further investigation and treatment of haematemesis, haemoptysis, anorexia and swelling at the ventral neck region. History revealed that the dog was abused by an individual who had pushed a wooden stick down to the throat through the mouth. The wooden stick piece (>20cm length) was removed through the oral cavity by the referring veterinarian, a day before presentation to UVH-UPM.
Upon presentation, the dog was quiet but alert and responsive, with rectal temperature of 38.9 ºC, pulse rate of 100 beats/min and respiratory rate of 20 breaths/min. Thoracic auscultation was not diagnostic as dog was panting. A slightly firm but painful soft tissue swelling was noticed around ventral neck area. Preliminary examination revealed sublingual haematoma and detailed inspection of the oral cavity was restricted because of the pain upon further oral manipulation. Abdominal palpation revealed no significant findings.
Diagnosis and treatment
A complete blood count (CBC) revealed marked neutrophilic leucocytosis (corrected white blood cell count: 46.1x109/L; reference range: 6–17x109/L, segmented neutrophils: 36.6x109/L; reference range: 3–11.5x109/L) with left shift (band neutrophil: 0.9x109/L; reference range: <0.3x109/L) and low thrombocyte count (195x109/L; reference range: 200–500x109/L). Meanwhile, serum biochemistry profile showed normal electrolytes, marked hyperglobulinaemia (67.9g/L; reference range: 25–45g/L), elevated alanine aminotransferase (136U/L; reference range: 5–90U/L) and alkaline phosphatase (288U/L; reference range, 40–100U/L).
Two orthogonal projections of the skull, neck (Figure 1) and thorax (images not provided) were taken. Lateral radiograph of the skull including neck revealed presence of a rounded soft tissue or fluid opacity structure with distinct margin located just ventral to the larynx, suggestive of soft tissue swelling or haematoma (Figure 1a). On both lateral and dorsoventral (DV) radiographs of the neck (Figure 1 b-d), multiple small rounded air opacities coalescing to linear gas opacities in bilateral fascial planes of neck were noticed. Left lateral view of the neck (Figure 1c) also indicates a cervical soft tissues emphysema ventral to laryngeal cartilages possibly secondary to oropharyngeal, laryngeal, oesophageal or tracheal perforation. Radiographic images of the thorax (images not provided) showed no significant finding, thus pneumomediastinum and mediastinitis were ruled out in preliminary examination.
Computed tomography (CT) scan of the neck region was acquired through cone beam CT scanner (Fidex; Animage LLC., Pleasanton, CA, USA) at 0.45–mm slice thickness. The anaesthesia was co-induced using 5mg/kg IV propofol and 0.2mg/kg IV midazolam administered to effect and
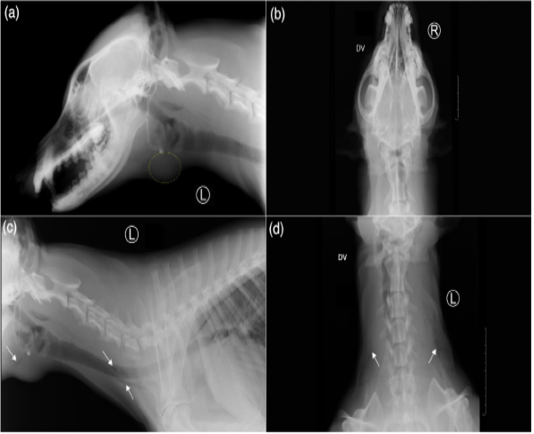
Figure 1: Radiographic views of the skull: left lateral (a) and dorsoventral (b), and the neck: left lateral (c) and dorsoventral (d) of the reported case. (a) There is presence of a rounded soft tissue or fluid opacity structure with distinct margin just ventral to the larynx (marked with yellow dotted circle). (c,d) On both left lateral and dorsoventral radiographs of the neck, multiple small rounded air opacities coalescing to linear gas opacities (white arrows), noticed in bilateral fascial planes of the neck indicating cervical soft tissues emphysema.
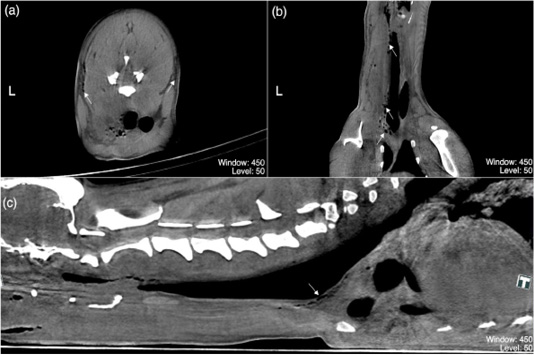
Figure 2: (a–c) are post-contrast multiplanar reformation (MPR) acquisitions of the neck region of the dog in present case study representing (a) transverse plane at the level of C5, (b) dorsal and (c) sagittal planes. Multiple small rounded gas-attenuating densities coalescing to form linear gas–attenuating densities peripheral to the fascial planes, oesophagus, and trachea (white arrows); indicating cervical soft tissues emphysema. Any piece of wood or splinter resembling structures were not identified from these CT acquisitions. (Window: 450; Level: 50)
maintained on 2% isoflurane. CT acquisitions using soft tissue window and level (W: 450 HU, L: 50 HU) revealed multiple small rounded air densities coalescing to linear gas–attenuating density at the periphery of the oesophagus and bilateral fascial planes of the neck, indicating cervical soft tissues emphysema (Figure 2 a–c). Any piece of wood or splinter resembling structures were not identified from the CT images.
Rigid transoral tracheoscopy revealed no abnormality, on the other hand esophagoscopy showed slight oedematous cranial oesophagus without any visible oesophageal perforation. Therefore, the dog was diagnosed with cranial oesophageal oedema possibly secondary to mild traumatic oesophageal perforation. Detailed secondary oral examination under general anaesthesia revealed prominent sublingual hematoma, yet to be resolved.
The dog was managed medically with an ancillary regimen of broad spectrum antibiotics to cover wide range of pathogenic bacteria, analgesics to cover pain, anti-emetic to stop vomiting reflux and antacids to reduce acidity in case regurgitating reflux happens. After 4 days of hospitalisation, the dog regained appetite and became brighter. Haematemesis and haemoptysis were resolved and the swelling under the ventral neck reduced to half of its size as compared to the initial presentation. The dog was discharged after 5 days of hospitalization with oral antibiotic for another 5 days and liver supplement for 7 days.
DISCUSSION
Oropharyngeal or oesophageal penetrating injuries are well characterised in dogs, which are commonly an unfortunate result of playing with wooden sticks (Doran et al., 2008). However, intraoral foreign object impalement, such as wooden stick would likely depict similar injuries, as described in the present case. Acute insult of <7 days would result in clinical signs such as oral pain, wounds, dysphagia, and haemoptysis. While in chronic cases of ≥7 days, clinical signs would direct towards recurrent abscessation and draining sinus tract at the neck and head region due to the retained foreign material (Griffiths et al., 2000). In present study the chronicity of the disease is acute in nature.
Initial management focuses on emergency respiratory and circulatory stabilisation, followed by detailed oral examination under general anaesthesia and survey radiography of the skull, neck and thorax as the primary imaging modality. The sites of gross intraoral injuries would allow the clinicians to determine the trajectory of the insult, thus providing extra information regarding the expectation of possible injuries of the anatomical structures deeper than the visible superficial lesions. Sublingual and lateral pharyngeal trajectories would result in less serious superficial injuries, while rostral pharyngeal trajectory may lead to deeper tissue injuries involving retrobulbar, temporal and masseteric region, and dorsal pharyngeal trajectory may cause retropharyngeal and oesophageal injury (Doran et al., 2008; Griffiths et al., 2000). Defensive struggling might be a possible explanation of multiple injuries related to sublingual and dorsal pharyngeal trajectories in this case.
Radiographic findings are often secondary to oropharyngeal or oesophageal perforation that include soft tissue swelling, cervical emphysema, pneumomediastinum, mediastinitis, and pneumothorax. Radiographical visualisation of wooden foreign material may not be possible as wood absorbs moisture from the saliva or wound environment, thus produces soft tissue opacity structure (Lamb et al., 2016). Furthermore, deeper soft tissue injuries are often undetectable or missed on plain radiography. Therefore, further investigation consisting of computed tomography, esophagoscopy and tracheoscopy are warranted to evaluate further assessment of possible deeper injuries, possible retained foreign material and potential surgical plan (Lamb et al., 2016). Radiological findings of this case are consistent with Lamb et al. (2016).
Radiographic evidence of cervical emphysema often influences the decision of surgical intervention; however, this remained debatable as several reports described successful management of oropharyngeal or oesophageal perforation with endoscopy and medical therapy in dogs (Robinson et al., 2014; Sterman et al., 2018; Teh et al., 2018). Endoscopy may serve diagnostic and therapeutic purposes as it allows direct visualisation of perforation and retrieval of foreign material in certain cases, respectively (Robinson et al., 2014). CT scan has been reported to have the sensitivity of 79% and specificity of 93% in the identification of wooden foreign body (Lamb et al., 2016), together with the ability of detecting deeper soft tissue injuries. In this case, no wooden foreign body was found in the CT scan, however gas attenuating densities suggested presence of gas in fascial planes of the neck region. Several clinicians prefer the use of contrast oesophagram to diagnose oropharyngeal or oesophageal perforation, however it carries the risk of mediastinitis due to leakage of contrast agent such as barium (Thompson et al., 2012).
In a previous study, oesophageal tears were repaired surgically with two layers simple interrupted sutures (Griffith et al., 2000). Surgical exploration may allow foreign material removal along with copious lavage and debridement of the perforated site, however medical management involving endoscopic retrieval may offer less invasive approach and shorter hospitalisation period. Recent records however focus on the medical management of oesophageal tears, and have reported a favourable outcome (Teh et al., 2018, Sterman et al., 2018). These reports suggest a spontaneous healing of the tissue, not requiring any surgical intervention. While, medical management includes administration of antibiotics, analgesics, and other symptomatic therapy if clinically necessary (Teh et al., 2018). In this particular case, absence of any foreign body constraint the clinicians to jump into surgical interventions and resolve the ailment successfully with medical management only. Integrative usage of CT and endoscopy may provide more information for the clinicians to select whether the case should be approached medically or surgically. However, decision-making in case management would vary according to the cost, skills, resources and severity of the injuries.
Conclusion
This report records the diagnosis of oesophageal penetration with the help of radiography and CT scan, along with its successful medical management. This is in the account of an acute oesophageal penetration, where surgical intervention was avoided, and the animal made a full recovery. Hence, clinicians shouldn’t be hurried to jump into surgical option provided patient is not deteriorating over period of time. A detailed timely screening of the affected areas would make a lot of difference in decision making process of the patient management. Furthermore, CT scan is a sensitive modality to screen the neck region for such penetrating cases.
acknowledgements
We would like to thank UVH-UPM staff for their support during this case management.
Conflict of Interest
The authors declare no conflict of interest.
authors contribution
LSF and PAMAR took part in the diagnostics of this case. All authors contributed to the writing and the revision of this manuscript.
REFERENCES






