Journal of Animal Health and Production
Case Report
Anal Reconstruction of Type II Atresia Ani in a 3-day Old Malin Lamb
Mohd Farhan Hanif Reduan*, Siti Nor Che Yahya, Nur Zul Izzati Mohd Rajdi, Rumaizi Shaari, Mimi Armiladiana Mohamad, Muhammad Luqman bin Nordin, Nurshahirah Shaharulnizim,*Intan Noor Aina Kamaruzaman
Faculty of Veterinary Medicine, Universiti Malaysia Kelantan, Pengkalan Chepa, 16100 Kota Bharu, Kelantan, Malaysia.
Abstract | This case reports highlights clinical and surgical management of Type II atresia ani in a 3-day old Malin lamb with a blind rectal pouch and slight abdominal distention. Anoplasty was performed to reconstruct the anal opening. Perineal skin tissue covering the anal opening was incised vertically and continued with blunt dissection to expose the blind end sac of the rectum. The blind rectum sac was retracted and excised, followed by a meconium evacuation. The rectal opening was secured to the perineal skin using multiple simple interrupted sutures. The animal recovered shortly without postoperative complications. Early surgical intervention is warranted in the atresia ani case to relieve the abdominal discomfort and preserve normal colonic activity, which was successfully attempted in this case.
Keywords | Atresia ani, Lamb, Anoplasty, Abdominal distension, Absent, Anal opening
Received | July 15, 2020; Accepted | August 05, 2020; Published | October 21, 2020
*Correspondence | Intan Noor Aina Kamaruzaman, Faculty of Veterinary Medicine, Universiti Malaysia Kelantan, Pengkalan Chepa, 16100 Kota Bharu, Kelantan, Malaysia; Email: [email protected]
Citation | Reduan MFH, Yahya SNC, Rajdi NZIM, Shaari R, Mohamad MA, Nordin ML, Shaharulnizim N, Kamaruzaman INA (2020). Anal reconstruction of type ii atresia ani in a 3-day old malin lamb. J. Anim. Health Prod. 8(4): 221-223.
DOI | http://dx.doi.org/10.17582/journal.jahp/2020/8.4.221.223
ISSN | 2308-2801
Copyright © 2020 Reduan et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Atresia ani is defined as a rare congenital deformity of the anus and rectum, which occasionally occurs in new-born animals. Although the condition is found in animals worldwide, atresia ani is rarely encountered in Malaysian livestock, possibly underreported. There are four types of atresia ani have been identified which are characterised by anal stenosis (Type I), imperforated anus with blind rectal pouch (Type II), or combined with more cranial termination of the rectum as blind pouch (Type III), and lastly, the discontinuation of the proximal rectum with the normal and terminal rectum (Type IV) (Vianna and Tobias, 2005). Atresia ani occurs as a result of incomplete development of urorectal fold to separate the cloaca of the hindgut or failure of the anal membrane to form an anal canal during embryonic development (Papazoglou & Ellison, 2012). The condition can occur in various animal species and most commonly reported in ruminants (Dennis & Leipold, 1972; Kiliç & Sarierler, 2004). Although atresia ani is a heritable condition, male animals are more affected than females, with higher prevalence being reported in the indigenous breed (72%) compared to crossbred (28%) in a previous study (Hossain et al., 2014). The diagnosis is based on the age, history, and physical examination of the perineal region, including digital palpation if the anal opening is present (Sutar et al., 2010) and accompanied by radiography for confirmation (Papazoglou & Ellison, 2012). Atresia ani can be corrected via surgical intervention, which is the goal treatment with variable prognosis (Kiliç & Sarierler, 2004). This case report highlights a case of atresia ani in a 3-day old lamb, which successfully treated via anal surgical reconstruction.
Case Details
A 3-day-old male Malin lamb was presented to the Veterinary Clinic of University Malaysia Kelantan, with the complaint of the absence of anal opening, no defecation, and distended abdomen, which were noticed after birth. General physical examination on the lamb exhibited normal vital parameters, except for slight abdominal distension and abnormal perineal region. An examination of the perineal area by digital palpation revealed a blind rectal pouch indented with an anal scar (~2 cm) (see Fig. 1A). The case was diagnosed as atresia ani (Type II or Type III), and anoplasty was planned to correct the condition.
The animal was placed in sternal recumbency and lignocaine hydrochloride 2% (w/v) was administered through caudal epidural as an anesthetic protocol. The surgical site was prepared by clipping the hair around the perineal area and cleaned using 4% (v/v) of chlorhexidine followed by 70% (v/v) of ethanol and lastly with 10% (v/v) of povidone iodine. An approximate 2 cm incision was made vertically on the anal scar and exteriorised the surrounding tissue by blunt dissection to retrieved for the rectal pouch (see Fig. 1B and 1C). The blind end of rectal tissue was retracted caudally to the perineal skin, and two stay sutures were placed opposite to one another on the perineal skin to hold the rectum sac (see Fig. 1D). The meconium was then evacuated through a small excision of the blind end of the rectum (see Fig. 1E). The now-exposed rectum sac was fixed around the perineal skin using multiple simple interrupted suture patterns (see Fig. 1F).
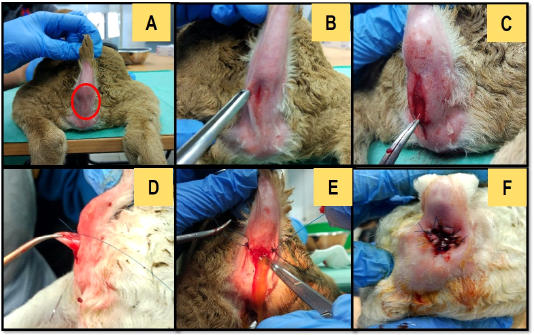
Figure 1: Anal surgical construction in a 3-day old Malin lamb in this case. A: Absence of rectal opening with an indented anal scar (mark with a circle). B: A vertical incision made on the anal scar. C: Blunt end dissection to retrieve anal sac. D: Anal sac retraction from the rectum. E: Two stay sutures placement on the perineal area and evacuation of meconium. F: Multiple simple interrupted sutures of anal sac fixed around the perineal area, exposing the anal opening.
Post-operatively, the lamb was given benacillin (1.0 ml/10 kg, IM, SID) as a prophylaxis antibiotic and flunixin meglumine (2.2 mg/kg, IM, SID) as analgesic and anti-inflammatory, respectively. The surgical site was sprayed using a fly repellent to prevent contamination. There was no post-complication observed, and the lamb was reported having a good appetite. Defecation was observed two days after the surgery, followed by suture removal after two weeks. The owner was advised to monitor abnormal signs such as faecal incontinence, tenesmus, and constipation. It was also advisable to not use the animal for breeding purposes in the future.
Discussion
The diagnosis of atresia ani can be made based on history, age, and physical examination. Additionally, radiographic examination and ultrasonography are considered ideal methods to confirm the rectal anomaly (Ellison, 2010). For example, the appearance of atresia ani in a plain radiograph may be visualised as gas-filled in the rectum and distal colon with a lack of colonic continuity, accompanied by the presence of fecalith in the distended part of the affected colon. Determination of the type of atresia ani will help the veterinarian in determining the position of the terminal rectum and use as an anatomical landmark during surgery.
Although no radiographic examination was available in this case, the case was confirmed as atresia ani Type II anomaly because 1) Absence of rectal opening and 2) No formation of anal fistula upon digital palpation and observed during surgery. New-borns with congenital atresia ani may survive up to 10 days following clinical signs such as depression, anorexia, colic, marked abdominal distension, thick white mucoid discharge from the anal region, and lack of faeces (Dreyfuss & Tulleners, 1989). Animals affected with Type II or III may die eventually due to bowel stasis if untreated. Anoplasty is the only treatment of choice to reconstruct the opening of the rectum to relieve abdominal discomfort whilst maintaining the function of the external anal sphincter, restoring colonic function, and preventing rectovaginal or urethrorectal connection (Suthar et al., 2010; Papazoglou & Ellison, 2012; Singh et al., 2018).
Generally, surgical correction of atresia ani in ruminant is recommended at earliest detection, preferably no less than a week old. Several techniques have been described previously depending on the types of anomaly, and the prognosis of surgery depends on the animal condition and the affected intestinal segment (Kiliç and Sarierler, 2004). Compare to small animals, ruminant has higher chances to survive the procedure with the number of case reports published elsewhere (Suthar et al., 2010; Saibaba et al., 2015; Mana et al., 2019). This is because, atresia ani is usually detected shortly after animals’ birth, and young ruminant usually can tolerate simple surgery at an early age compared to small animals that require invasive surgery at 6-8 weeks of age (i.e. abdominal exploratory or colostomy) that poses high anaesthetic risks.
Postoperative complications of anal surgery that include recto-anal structure formation, faecal incontinence, constipation, and megacolon (Williams, 2005). These effects, however, are more pronounced in small animals compared to ruminants. Additionally, anal stenosis may occur due to improper suture techniques during surgery. The prognosis of the animal in this case was good without life-threatening complications. Animals with a history of atresia ani or other congenital anomalies are not recommended to be used for breeding due to the possibility of genetic inheritance (Smith and Sherman, 2009).
Conclusion
Atresia ani is a congenital anomaly of a new-born animal that can be managed via surgical repair. Prompt diagnosis is crucial to determine the type of atresia ani anomaly. Early surgical intervention is warranted to relieving the abdominal discomfort, preserving normal colonic activity to improve the animals’ quality of life, which was successfully attempted in this case.
Conflict of interest
The authors declare that there is no conflict of interest.
Authors’ contribution
Siti Nor Che Yahya, Nur Zul Izzati Mohd Rajdi, Rumaizi Shaari, Mimi Armiladiana Mohamad and Nurshahirah Shaharulnizim for diagnosing and performing the surgery. Intan Noor Aina Kamaruzaman, Mohd Farhan Hanif Reduan, and Muhammad Luqman bin Nordin for preparing and reviewing the manuscript.
Acknowledgement
The authors wish to appreciate the staff of Universiti Malaysia Kelantan Veterinary Clinic for their technical assistance during the handling of this case.
References






