Journal of Animal Health and Production
Research Article
Effect of Autologous Plasma Treatment on the Cornea Regeneration with Keratoconjunctivitis Sicca in Dogs
Yury Anatolyevich Vatnikov¹, Ilya Sergeevich Erin¹, Suleiman Mukhitdinovich Suleimanov², Evgeny Vladimirovich Kulikov¹, Sergey Borisovich Seleznev¹, Vladimir Ivanovich Lutsay³, Irina Anatolyevna Popova¹*, Aleksandr Anatolyevich Strizhakov¹, Ilya Fedorovich Vilkovysky¹
¹Peoples’ Friendship University of Russia (RUDN University). Moscow, st. Miklukho-Maklaya, 6, 117198; ² Voronezh State Agrarian University named after Emperor Peter I, Voronezh, st. Michurina, 1, 394087; ³ Moscow State University of Food Production. Moscow, st. Vrubel, 12, 125080.
Abstract | Our study was aimed at assessing the effectiveness of autologous plasma enriched with platelets as part of the complex treatment of keratoconjunctivitis sicca (KCS) of moderate severity in dogs. In our experiment, 20 dogs of various breeds with clinical signs of keratoconjunctivitis sicca participated. The animals were divided into the experimental group and the control group, 10 dogs in each group. The animals of the control group were treated with standard treatment: local antibiotic therapy, a topical immunosuppressant (cyclosporine), and also a lubricant. In addition to standard treatment, an autologous platelet rich plasma (PRP) was additionally subconjunctivally injected weekly to animals of the experimental group. The effectiveness of the treatment was evaluated by monitoring the changes in the hydration level of the anterior segment of the eye, the cytological picture of smears and gross anatomical appearance of the front of eye. The results in experimental group demonstrated a decrease in the number of desquamated epithelial cells, as well as a more intense decrease in segmented cells. The dynamics of the reduction of the clinical manifestations of KCS in animals that used PRP as part of complex therapy is more pronounced and was quite fast. Our observations show that autologous platelet-rich plasma is a powerful protector of corneal regeneration and therefore could be recommended to use in corneal erosion, keratitis ulcers and corneal injuries, as well as a keratoprotector after surgical interventions on the cornea and intraocular structures.
Keywords | Keratoconjunctivitis sicca, Autologous platelet-rich plasma, Subconjunctival injection, Cornea, Dog.
Received | June 20, 2019; Accepted | September 02, 2019; Published | February 01, 2020
*Correspondence | Irina Anatolyevna Popova, Peoples’ Friendship University of Russia (RUDN University). Moscow, st. Miklukho-Maklaya, 6, 117198; Email: [email protected]
Citation | Vatnikov YA, Erin IS, Suleimanov SM, Kulikov EV, Seleznev SB, Lutsay VI, Popova IA, Strizhakov AA, Vilkovysky IF (2020). Effect of Autologous Plasma Treatment on the Cornea Regeneration with Keratoconjunctivitis Sicca in Dogs. J. Anim. Health Prod. 8(1): 1-7.
DOI | http://dx.doi.org/10.17582/journal.jahp/2020/8.1.1.7
ISSN | 2308-2801
Copyright © 2020 Popova et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Currently, the problem of eye diseases in small pets is quite acute (Kim et al., 2016; Erin et al., 2017; de Queiroz et al., 2018; Kirschweng et al., 2018). Inflammatory diseases of the anterior segment of the eye, cornea, and conjunctiva occupy a major place in the practice of a veterinary ophthalmologist (Wilmis, 2007; Martin-Alarcon and Schmidt, 2016; Temple-Wong et al., 2016). Keratoconjunctivitis sicca (KCS) in dogs is a dysfunction based on a violation of tear production (Aicher et al., 2015; Kim et al., 2015; Lee et al., 2015; Vatnikov et al., 2015; Wilmis, 2007). KCS is a polyetiological disease characterized by manifestations of corneal conjunctival xerosis (Esson, 2015; Meng et al., 2015; Tseng et al., 2015; Krasnikov et al., 2016) associated with impaired hydration of the anterior segment of the eyeball (cornea and conjunctiva) (Wilmis, 2007; Kulikov et al., 2017; Stern et al., 2017). KCS is accompanied by the following clinical signs: conjunctival hyperemia, eye discomfort (Tabery, 2012; Kim et al., 2016), pain, corneal vascularization, corneal pigmentation, and the appearance of profuse mucopurulent discharge (Tseng et al., 2015; Jonsson et al., 2018). KCS may also cause, secondary diseases including conjunctivitis, vascular and pigment keratitis, erosion and xerotic corneal ulcers (Pflugfelder et al., 2017; Williams et al., 2017). KCS can affect both one eye and both, and the degree of damage to both eyes will not always be the same (Mitrokhina et al., 2014; Gronkiewicz et al., 2017; Yang et al., 2017). KCS treatment can be conservative or surgical, and often combine these two methods (Jonsson et al., 2018). In the treatment of KCS, it is recommended to prescribe immunosuppressive drugs for a long time, and limited results with side effects are often noted (Dunn, 2014; Braidee et al., 2018).
Platelet-rich plasma (PRP) is a plasma taken from a particular patient, which contains an increased number of growth factors, which evidenced by an increased platelet count after centrifugation. PRP contain growth factors which play a very important role in tissue regeneration, angiogenesis and proliferation (Lubkowska et al., 2012). Autologous platelet rich plasma is a fibrin network that supports the regenerative matrix. Its’ use may enhance the differentiation of cells, stimulate regeneration and angiogenesis, thereby accelerating the healing processes of various injuries (Pflugfelder et al., 2017; Yang et al., 2017).
Keeping in view the biological activities of PRP, the current study was designed with the aims to assess the effects of platelet-rich autologous plasma treatment on corneal regeneration in keratoconjunctivitis sicca of moderate severity in dogs.
Materials and methods
Ethical Approval
The present study was carried out in accordance with the State program of Peoples’ Friendship University of Russia (RUDN University). Selective research on animals was conducted after receiving approval of Bioethics commission SREC PFUR.
Experimental Animals
We examined 20 dogs (40 eyes) with moderate KCS symptoms. The animals were divided into 2 groups: an experimental group and a control group, 10 animals each. All animals of the experimental and control groups showed clinical signs of KCS in at least one eye (mucous or mucopurulent discharge, conjunctival hyperemia, corneal neovascularization and its clouding). The animals of the experimental group received treatment based on platelet rich plasma (PRP), and the animals of the control group received the usual standard treatment.
Obtaining Autologous Platelet Rich Plasma
Before taking venous blood, the animals were kept on a starvation diet for at least 12 hours. Blood was taken from the saphenous vein of the forearm into special tubes for plasmolifting. Venipuncture was performed using a VASOFIX catheter (BBRAUN, Germany). The diameter of the catheters ranged from 22G (0 0.9 mm) to 18G (about 1.3 mm), depending on the individual diameter of the animals’ veins. After the blood sampling procedure, the blood tube was turned over several times so that the whole blood mixes with the anticoagulant. Then centrifuged for 10 minutes at a speed of 1500 rpm. After centrifugation, the contents of the tube were divided into 3 layers: the upper liquid of yellowish-straw color (autologous platelet rich plasma), the middle layer is a separation gel, and the lower one is reddish-red blood cell clot (Marx, 2004; Akhmerovet al, 2011; Kovach et al, 2014).
Research Design and Methodologies Used
As follows from the Table 1, the animals of the experimental group received antibiotic ciprofloxacin (eye drops of ciprovet) as therapy, cyclosporin A (ophthalmic ointment Optimun) was used as an anti-inflammatory drug, and a lubricant based on dexpanthenol (cornegel) was used as a moisturizing drug. Injections of physiological NaCl 0.9% in a volume of 0.3 ml were carried out for the purity of the experiment, only in order to cause the same changes in the animals of the experimental and control groups associated with the injection procedure itself. The treatment of animals of the experimental group was identical, except that they used subconjunctival administration of PRP once a week. The experiment was held for 8 weeks.
The initial data according to Shirmer tear test (STT) (Kim et al., 2016), which we performed at the initial intake, coincide in the animals of the experimental and control groups (10±0.19 mm/min). Conjunctivitis sicca of moderate severity is characterized by a level of tear production of 8-10 mm / min (Meng et al., 2015; Kim et al., 2016). Based on the dynamics of changes in the level of tear production, we compared the effectiveness of treatment without the use of PRP and with the use of PRP.
To compare the effectiveness of treatment with and without PRP, we used the following methods: Visual examination of sick animals using optical instruments (Heine binocular magnifier, Karl Zeiss surgical microscope), corneal biomicroscopy, ophthalmoscopy of the fundus and cornea using direct ophthalmoscope (Rudolf Riester company, Jungengen, Germany) and indirect ophthalmoscope (Appasamy Associates, Chennai, India). In addition, the fluorescein test was done using a blue cobalt filter and Schirmer’s tear test (STT) according to Cherry et al. (2018). Material was taken for cytological studies using the smear-imprint method i.e., gently touching of glass slide to the surface of the cornea of the eye (Tabery et al., 2012; Kim et al., 2016). Slides with pathological material were dried in air at room temperature and stained using the Diff-Quick method (Tabery et al., 2012; Kim et al., 2016). Further study of the smears was carried out using a biomed-6 trinocular laboratory microscope (St. Petersburg, Russia). under high and low magnifications. For clarity of the cytological picture in the dynamics of the treatment of the disease, we took photographs of micropreparations.
Statistical Analysis
The digital material was subjected to mathematical processing using the software package Statistica 6.0.
Results and discussion
To assess the short-term effect of the use of autologous platelet-rich plasma, STT was used and a visual assessment of the ocular surface was performed. STT was performed directly on the day of initial administration, after 30 days, and after 60 days. Simultaneously with the examination and STT, material was taken for cytological examination. Cytology was also performed on day 1, day 30, and day 60 of the experiment. According to Shilkin et al. (2017) the use of PRP is a proven method for the treatment of ulcers and erosion of the cornea of various origins, as well as a method of accelerating regeneration during corneal transplants. Our data showed that the plasma lifting method is safe, since we did not observe any side effects during the experiment. In all animals from the experimental group with an average degree of KCS, STT and cytology data returned to the physiological norm of healthy animals. The animals of the control group also showed the presence of positive dynamics, but these changes were less intense.
In animals of the control group that received standard treatment, the dynamics was also positive, but less intense. Animals with KCS of moderate severity (tear production level of 10 ± 0.19 mm / min) after 30 days of treatment had STT results of 13 ± 0.99 mm / min, which corresponds to KCS of moderate severity; while after 60 days of treatment, the level of tear production was quite close to physiologically normal and was 15 ± 1.3 mm / min, such STT values were maintained until the end of the experiment (Table 2). At the same time, in animals from experimental groups, the dynamics of changes in the level of hydration of the anterior ocular surface was more intense. It has been scientifically proven that with dry keratoconjunctivitis there is an urgent need for frequent topical use of tear fluid substitutes, but at the same time, the preservatives contained in these preparations can have a toxic effect on the corneal and conjunctival tissues (Yingfang et al., 2016; Erin et al., 2017; Stern and Pflugfelder, 2017). In dogs, whose level of tear production was 10 ± 0.19 mm / min, which corresponds to KCS of moderate severity, by the 30th day of treatment it rose to 18 ± 1.3 mm / min, which corresponds to healthy animals and this level of moisture remained until the end of the experiment. Based on the data presented, it can be concluded that the plasma lifting method as part of complex therapy promotes the regeneration of corneal and lacrimal gland tissues, and the level of moistening of the anterior segment of the eye (conjunctiva and cornea) increases.
It can be assumed that the presence of growth factors in PRP helps to improve the susceptibility of corneal tissue and dog conjunctiva to drugs (Table 1). Based on this, it is possible to recommend the use of PRP in such pathological processes as dry keratoconjunctivitis, keratitis of various etiologies, corneal ulcers, corneal dystrophy, chemical and thermal burns of the eyes, corneal worms, chronic persistent defects of the epithelium and stroma of the cornea. The level of total tear production is restored in more complete volume by the 6th week of treatment using PRP. Remission is persistent, but subject to constant symptomatic therapy.
Table 1: Treatment regimens for keratoconjunctivitis sicca in dogs of the control and experimental group
| Group 1 (control) | Group 2 (experimental) |
|
1. Ciprovet (eye drops): 3 times a day 2.Optimune (eye ointment Cyclosporin A): 3 times a day 3.Corneregel: 3 times a day 4.NaCl 0.9%: 0.3 ml subconjunctival once a week |
1. Ciprovet (eye drops): 3 times a day 2.Optimune (eye ointment Cyclosporin A): 3 times a day 3.Corneregel: 3 times a day 4. PRP*: 0.3 ml subconjunctival once a week |
*PRP: platelet rich plasma
The dynamics of corneal regeneration in animals of the control group with moderate keratoconjunctivitis sicca is as follows: at the initial intake in these animals, the cornea was not transparent due to edema, and the presence of abundant pigment (Figure 1). In case of damage or inflammatory processes in the cornea, the arrangement of collagen fibers is reorganized, while they are saturated with moisture, swell and the cornea may lose its transparency, which leads to decreased vision (Aicher et al., 2015; Tseng et al., 2015). Abundant mucopurulent discharge was observed, and the high cellularity of smears was determined cytologically, the background was represented by mucus, epithelial cells and cells of the leukocyte series, mainly segmented neutrophils, were found among the cells (Figure 2). After 30 days of treatment using standard methods (Table 1) in animals of the control group with keratoconjunctivitis sicca of moderate degree, the cornea did not become more transparent, but at the same time acquired smoothness, its surface became shiny. Cytology after 30 days determined the high cellularity of the smear, the cellular composition was represented by epithelial cells and segmented cells in large numbers, which indicates the presence of a severe inflammatory process (Figure 2). By the 60th day of treatm-
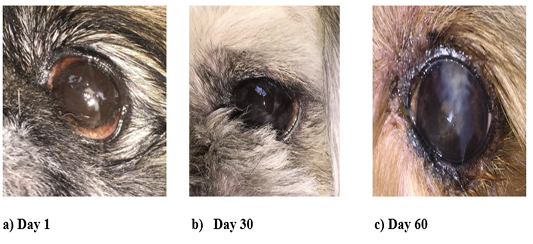
Figure 1: Visual changes in the anterior surface of the eye in animals of the control group with moderate KCS
ent, the cornea of the animals of the control group with moderate KCS became partially transparent, due to the reduction of edema and partial resorption of melanin, the pupil and iris, as well as the lens, could be visualized. The cytological picture was not much different from the previous one. The smear cellularity was also increased and represented by epithelial cells and leukocytes (Figure 2).
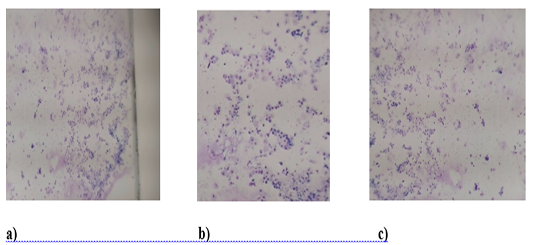
Figure 2: Cytology of the front surface of the eye in animals of the control group with moderate KCS. a) (Day 1), b) (Day 30) and c) Day 60, have over 50 cells each (epithelial cells and segmented cells). The background is slimy.
The dynamics of corneal regeneration in animals of the experimental group with moderate keratoconjunctivitis sicca was more intense: at the initial intake in these animals, the cornea was not transparent due to edema, and the presence of abundant pigment (Figure 3). Abundant mucopurulent discharge was also observed, while the cytological picture was characterized by high cellularity of smears, the background was represented by mucus, epithelial cells and cells of the leukocyte series, mainly segmented neutrophils, were found among the cells (Figure 4). After 30 days of treatment using PRP in animals of the experimental group with moderate keratoconjunctivitis sicca, the cornea became more transparent by reducing edema and resorption of melanin, while acquiring smoothness, its surface became shiny. By cytology after 30 days a low smear cellularity was determined, the cellular composition was represented by a moderate number of epithelial cells and segmented cells. By the 60th day of treatment, the cornea of the animals from the experimental group with moderate KCS became transparent, due to the reduction of edema and resorption of melanin, the pupil and iris, as well as the lens, could be visualized. The cytological picture was as follows: the cellularity of the smears is not high and is represented by a small number of epithelial cells and lymphoid cells also in a small amount (Figure 4).
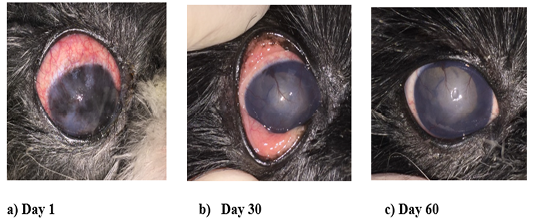
Figure 3: Visual changes in the anterior surface of the eye in animals of the experimental group with moderate KCS
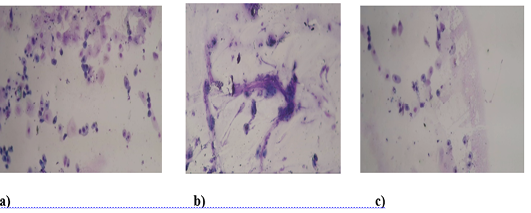
Figure 4: Cytology of the anterior surface of the eye in animals of the experimental group with moderate KCS. a) Day 1. High cellularity. It is mainly represented by epithelial cells and segmented cells. b) Day 30. Mucous background, cellularity moderate. Epithelial cells and segmented cells are presented. c) Day 60. Cellularity is not high. Mostly epithelial cells.
From the data presented, it can be concluded that the use of autologous platelet-rich plasma as part of complex therapy for dry keratoconjunctivitis of dogs of moderate severity is more effective compared to the generally accepted methodology (Table 1), which expressed a more intensive increase in the level of moistening of the anterior surface of the eye and more intense processes of regeneration of the cornea (Table 2).
Table 2: The results of STT (Shirmer tear test) in animals of the experimental and control group
| Groups | Day 1 | Day 30 | Day 60 |
| Group 1 (Control) | 10±0.19 mm/min | 18±1.3 mm/min | 18±1.6 mm/min |
| Group 2 (Experimental) | 10±0.19 mm/min | 13±0.99 mm/min | 15±1.3 mm/min |
A significant number of CKS treatment methods reflect the efforts of researchers and clinicians to exert a therapeutic effect on the links of the pathological process. Almost all approaches to the treatment of keratoconjunctivitis sicca in dogs are reduced to the use of immunosuppressants, such as glucocorticosteroids, cyclosporin-A and tacrolimus (Martin-Alarcon and Schmidt, 2016; Yingfang et al., 2016; Erin et al., 2017; Stern and Pflugfelder, 2017; Williams and Tighe, 2018). Unfortunately, preparations based on artificial or natural tears require an increased frequency of instillations (up to 8 times per day), which is not always possible. In our opinion, the existing methods of conservative treatment of CKS in dogs are not effective enough and the improvements are only temporary.
To date, autologous platelet-rich plasma is used in many branches of medicine (Esson, 2015; Tsubota et al., 2017; de Queiroz et al., 2018; Cherry et al., 2018). Unfortunately, the use of PRP in veterinary medicine does not find such widespread use. The role of platelets in hemostasis is most widely known, in addition to the fundamental role in the process of blood coagulation, platelets have other features. Platelets contain proteins that play an important role in tissue regeneration. These proteins are called growth factors, which play a key role in regenerative processes. In PRP, these growth factors are present in large quantities. The presence of growth factors allows the use of PRP as a stimulator of tissue regeneration (Sherer and Tobalem, 2012; Yang et al., 2016; Pflugfelder et al., 2018; Oliveira et al., 2019). In domestic and foreign literature, data on the use of autoplasma are not quite complete, therefore, we believe that the use of autoplasma enriched with platelets in veterinary medicine is a very promising method. The method consists in collecting venous blood, followed by centrifugation. The issue of methods for obtaining PRP is quite debatable and represents a huge field for activity. In our opinion, the method of single slow centrifugation is of scientific and practical interest.
The high incidence of KCS among dogs and the imperfection of existing methods of treatment allows clinicians to test and search for new methods of treating this disease directly in sick animals, without using laboratory animals. As drugs of choice in the treatment of inflammatory diseases of the cornea, we recommend eye drops or ointments containing ciprofloxacin and gentamicin in their composition for stopping the development of microflora in combination with glucocorticosteroids. It can be assumed that the presence of growth factors in PRP improves the susceptibility of dog corneal tissue and conjunctiva to drugs. Based on this, it is possible to recommend the use of PRP in such pathological processes as keratoconjunctivitis sicca, keratitis of various etiologies, corneal ulcers, corneal dystrophy, chemical and thermal burns of the eyes, corneal worms, chronic persistent defects of the epithelium and stroma of the cornea. The level of total tear production is restored in more complete volume by the 6th week of treatment using PRP. Remission is persistent, but subject to constant symptomatic therapy.
Comparison of modern treatment regimens and regimens with the addition of autologous platelet-rich plasma has shown sufficient therapeutic efficacy of the latter in the treatment of keratoconjunctivitis sicca in dogs and associated erosion and xerotic ulcers on the cornea of the eye. When using autologous plasma as part of the complex therapy of KCS, the treatment time is reduced, the frequency of instillation of antibiotics, immunosuppressive drugs is reduced, the period of remission is prolonged, which is persistent and long. Based on the results of our study, dogs that showed moderate KCS, receiving autologous platelet-rich plasma as part of complex therapy, had more intense positive dynamics and by the 30th day of treatment the degree of hydration of the anterior segment of the eye was normal. Against the background of standard treatment using generally accepted methods of therapeutic effect, the level of hydration of the anterior segment of the eye also increased, but the positive dynamics were less intense and less pronounced. Our studies in the field of application of PRP in veterinary ophthalmology show that the level of general tear production in moderate KCS is restored faster and in a larger volume, in comparison with standard conservative treatment methods.
Conclusion
Based on our data, it could be concluded that autologous platelet-rich plasma has a key role in tissue regeneration in dogs suffering from moderate KCS. Thus, its’ use could be recommended in various types of inflammatory or traumatic processes in the tissues of the anterior ocular surface of animals.
Acknowledgments
This paper was financially supported by the Ministry of Education and Science of the Russian Federation on the program to improve the competitiveness of Peoples’ Friendship University of Russia (RUDN University) among the world’s leading research and education centers in the 2016-2020. The publication was prepared with the support of the “RUDN University Program 5-100” (the agreement number 02.a03.0008).
Conflict of interest
We declare that authors have no competing interest.
Authors contribution
The authors contributed equally.
References






