Research Journal for Veterinary Practitioners
Case Report
Primary Retrobulbar and Intraocular Malignant Melanoma in a Cat
Jedsada Siripoonsub1, Katriya Chankow2, Sitthichok Lacharoje3, Anudep Rungsipipat1*
1Companion Animal Cancer Research Unit, Department of Pathology, Faculty of Veterinary Sciences; 2Small Animal Teaching Hospital, Faculty of Veterinary Sciences; 3Department of Pathology, Faculty of Veterinary Sciences, Chulalongkorn University, Bangkok-10330, Thailand.
Abstract | Retrobulbar and intraocular melanoma in cats is infrequently described. The objective of this report is to describe the macroscopic, histopathological and immunohistochemical findings of intraocular and retrobulbar malignant melanoma in a cat. A 10-year-old, spayed female, domestic short hair cat presented a rapidly growing intraocular and retrobulbar mass affecting the right eye. The presence of this mass resulted in exopthalmos, blindness and multifocal hemorrhage. The cat died 4 weeks later and a complete necropsy was performed. The final diagnosis for this case was primary retrobulbar malignant melanoma with intraorbital involvement. Most of the feline intraocular tumors contained a tumor that are predisposed to trauma due to inflammation. Early enucleation is the treatment of choice for malignant melanocytic tumors and for blind or painful eyes.
Keywords | Cat, Intraocular, Melanoma, Retrobulbar
Editor | Muhammad Abubakar, National Veterinary Laboratories, Islamabad, Pakistan.
Received | March 01, 2016; Revised | March 20, 2016; Accepted | March 23, 2016; Published | April 27, 2016
*Correspondence | Anudep Rungsipipat, Companion Animal Cancer Research Unit, Department of Pathology, Faculty of Veterinary Sciences, Chulalongkorn University, Bangkok-10330, Thailand; Email: anudep.r@chula.ac.th
Citation | Siripoonsub J, Chankow K, Lacharoje S, Rungsipipat A (2016). Primary retrobulbar and intraocular malignant melanoma in a cat. Res. J. Vet. Pract. 4(2): 25-29.
DOI | http://dx.doi.org/10.14737/journal.rjvp/2016/4.2.25.29
ISSN | 2308-2798
Copyright © 2016 Siripoonsub et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Melanomas are tumors of melanoblasts and melanocytes, which can have a benign or malignant clinical course. They may occur on the skin, in the oral cavity or be associated with the eye. Malignant melanoma is the most common primary intraocular tumors in cats (Paridaens et al., 1994; Day and Lucke, 1995; Luna et al., 2000). The most common site of primary malignant melanoma in cats is reported to arise in the eye; (intraocular), followed by the skin and the oral cavity. This is in contrast to what is seen in dogs. Ocular melanomas are designated, in accordance with three main locations, as epibulbar (limbal), uveal, or conjunctival. Melanomas in other sites in the feline eye (e.g. limbal, conjunctival) are sporadically reported. The limbus is the most common of these sites, followed by the conjunctiva (Payen et al., 2008). Limbal (epibulbar) melanoma arises from the neural crest melanocytes of the limbus, deep in the sclera. Limbal melanomas are smooth and darkly pigmented neoplasms that arise from the melanocytes normally encountered in the corneoscleral junction of dogs and cats, and extend both anteriorly and posteriorly involving the corneal stroma and/or sclera.
In cats, iridial melanomas develop from the anterior uvea (iris and ciliary body) with diffuse iris melanoma being the most common variant. Sometimes, extension to the peripheral choroid, a transcleral extension, or infiltration of the iridocorneal angle with secondary glaucoma may occur (Schobert et al., 2010; Semin et al., 2011). Incidence of metastasis of iridial melanomas in cats is high, while that of tumors arising from the conjunctiva and limbus is rare (Grahn et al., 2006). Decrease in survival time occurs when the diffuse iris melanoma reaches the ciliary body stroma, and metastatic disease occurs in approximately 30-50% of affected feline patients (Semin et al., 2011).
This report describes the macroscopic, histopathological findings and immunohistochemical properties of intraocular and retrobulbar malignant melanoma in a cat.
A 10-year-old, spayed female, domestic short hair (DSH) cat was presented at the Oncology clinic, Small Animal Teaching Hospital, Faculty of Veterinary Science, Chulalongkorn University, Bangkok, Thailand with a rapidly growing intraocular and retrobulbar mass affecting the right eye. Upon physical examination, the right eye was infiltrated and partially replaced by a 1x2 cm, pale pink retrobulbar mass. The presence of the mass resulted in exopthalmos, blindness and multifocal hemorrhage. The menace response was absent, and the direct and consensual pupillary light responses were sluggish. The left eye demonstrated normal reflexes with uveal hyperpigmentation. The abnormality was discovered initially on a routine physical examination, at which time a tentative diagnosis of ocular melanoma was made. Frontal radiography revealed right orbital swelling with zygomatic bone lysis and concurrent bronchopneumonia. The cat died 4 weeks later and a complete necropsy was performed.
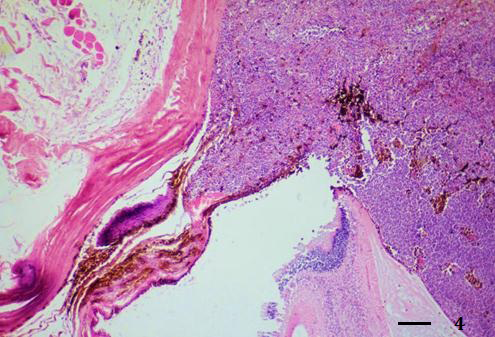
The cat was submitted for necropsy at the Department of Pathology, Faculty of Veterinary Science, Chulalongkorn University. Upon necropsy, a firm large brown to black retrobulbar and intraocular mass was effacing the anterior and posterior chambers of the right eye (Figure 1, 2 and 3). No evidence of tumor mass metastasis in visceral organs was observed and the other organs had no remarkable changes.
The affected eye, brain, lung, heart, spleen, kidney, liver, lymph node and gastro-intestinal tract were preserved in 10% neutral buffered formalin for histopathology. The samples were underwent routine histologic procedure, embedded in paraffin, and were sectioned at 4-6 um thickness. The sagittal sections were routinely stained with Hematoxylin and Eosin (H&E) and observed under light microscope. To highlight melanin pigments within the mass, additional stains including Periodic Acid Schiff (PAS) and Masson Fontana (MF) were performed in the right eye sections without prior depigmentation.
Moreover, immunohistochemistry was also performed on the affected ocular section by LSAB method with Melan-A antibody. In brief, paraffin-embedded sections were obtained. Heat-induced epitope retrieval with citrate buffer, pH 6.0, was performed for 5 minutes at 1210C followed by endogenous peroxidase blocking with 3% hydrogen peroxide and incubation with the primary antibody at 40C for 10 hours. A pre-diluted monoclonal mouse anti-MART-1/ Melan-A (clone A103, dilution 1/100, Dako, Denmark) was used as a primary antibody. A dual link Envision Polymer (Dako, Denmark) and 3, 3’- diaminobenzidine kit were used to detect the immunoreactive complexes. The slides were then counterstained with Mayer’s hematoxylin. Intense brown intracytoplasmic staining in the neoplastic cells was recognized as positive cells.

Figure 3a:Firm large brown to black retrobulbar and intraocular mass effacing both anterior and posterior chambers of the right eye (Figure 3A)

Figure 3b: compared to normal left eye (Figure 3B)
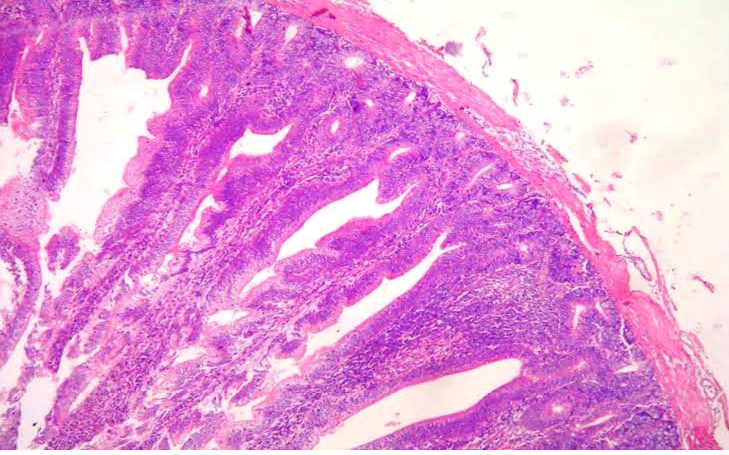
The neoplastic cells were arranged in a dense palisading pattern of epithelioid cells which appeared to have originated from the iris and subsequently invaded the periocular tissue (Figure 4). Neoplastic cells were large and spindaloid had large ovoid nuclei and contained brown to black intracytoplasmic pigments consistent with melanin (Figure 5 and 6). Fibrozing keratitis affected the cornea. Masson Trichrome staining showed intense black granules, consistent with melanin in the cytoplasm of the tumor cells while stained negative with PAS. Melan-A protein expression was assessed and the neoplastic cells demonstrated strong cytoplasmic immunoreactivity (Figure 7).
The final diagnosis based on gross, histopathology and immunohistochemistry of this case was primary retrobulbar malignant melanoma with intraorbital involvement.
Intraocular melanoma in cats is infrequently described compared to canine melanocytic tumors. This neoplasm arises from the choroid and occurs in approximately 5% of the frequency of anterior uveal melanoma, and is also generally considered as benign (Semin et al., 2011). The main
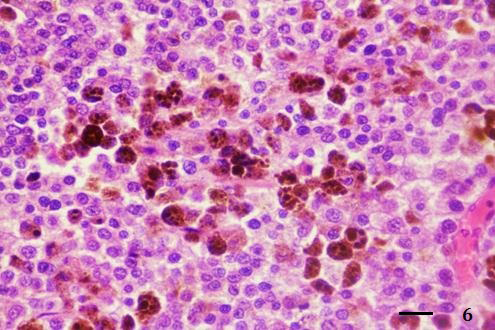
Figure 6: Neoplastic cells had large epithelioid shape and contained intracytoplasmic brown black melanin pigments (H&E stain, bar = 25 µm)
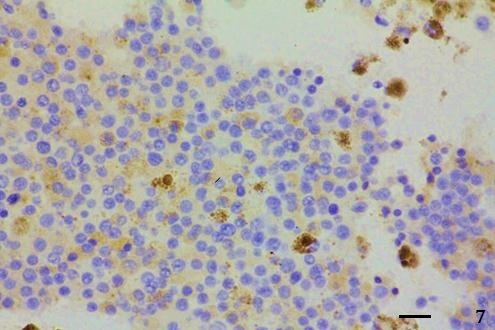
Figure 7: Tumor cells showed intense cytoplasmic Melan-A protein expression (IHC; Envision polymer, counterstained with Mayer's Hematoxylin, bar = 25 µm)
criteria used to distinguish benign from malignant forms are histologic features including nuclear atypias, mitotic index, and tumoral cell type. Orbital and retrobulbar tumors are occasionally observed in cats and dogs. They can be characterized as primary, when arising from any tissues that compose and surround the orbit, or secondary when resulting from orbital extension of tumors of the globe or optic nerve, the nasal cavity or paranasal sinuses, the salivary glands, or orbital involvement by systemic neoplasia (de Lorimier, 2006). This present case was diagnosed as primary retrobulbar malignant melanoma with intraorbital involvement based on these criteria.
Ocular melanomas are tumors that tend to occur in the anterior uveal tracts of felines; originating within the iris which was the most likely origin in this cat since it was affecting the anterior chamber (Cagnini et al., 2012). In humans, congenital ocular and oculodermal melanocytosis are the predisposing conditions commonly associated with uveal melanoma, however, there have been no reports in animals (Gunduz et al., 1998). The etiology of feline conjunctival melanomas due to the predilection for the superior bulbar location in cats may suggest ultraviolet radiation exposure, as is suspected in humans. Recent data suggest that conjunctival melanomas are associated with premalignant acquired melanosis, a premalignant flat and variably brown unilateral lesion showing cellular atypia (Payen et al., 2008).
Uveal melanocytomas are composed of a variable proportion of heavily pigmented spindle cells and non-cohesive heavily pigmented plump polyhedral cells with minimal anisokaryosis and anisocytosis. In cats, the classical clinical presentation is a diffuse iridial melanoma with progressive focal area of iris pigmentation that gradually becomes a coalescent-infiltrating lesion affecting the iris stroma. In advance cases, tumor cell dispersion can lead to glaucoma by iridocorneal angle obstruction. Local extension may affect other ocular structures such as ciliary body, adjacent choroid, and sclera (Bourguet et al., 2015). Ocular melanoma results in significant thickening of the uveal structures and anterior sclera due to infiltration by pigment-laden melanocytes, and to a lesser extent melanophages. Secondary glaucoma may subsequently occur due to impedance of the aqueous outflow by pigment (Dees et al., 2013).
Most of the feline intraocular tumors, including uveal melanoma and lymphoma, had associated lens rupture in previous reports by Garhn et al. (2006). It indicated that feline eyes containing a tumor are predisposed to trauma or self-trauma due to inflammation induced by the tumor. This might support the hypothesis that inflammation precedes the development of a tumor and may induce intraocular neoplastic transformation (Grahn et al., 2006).
The differential diagnoses for this neoplasm include round cell tumors such as lymphoma and histiocytoma. Immunohistochemical staining with specific Melan-A permitted a more definitive diagnosis. The ocular melanoma in this case is suspected to have originated from the pigmented iridial epithelium, which represents the most common site of melanocytic, neoplastic transformation in the feline eye. Melan-A is an immunohistochemical marker that has been evaluated in cats on formalin-fixed tissue; it was shown in one report to be positive in 67% of feline melanomas (Ramos-Vara et al., 2002). Immunohistochemistry has shown that the pigment-laden cells in ocular melanoma are usually positive for vimentin, S100, neuron- specific enolase, and Melan-A and negative for cytokeratin (Dees et al., 2013).
For large intraocular tumors or those with metastatic potential, enucleation may be considered the best option (Dees et al., 2013). Metastatic rates for cutaneous melanomas in cats have been reported to range from 5 to 25% (Patnaik and Mooney, 1988). Intraocular melanomas are thought to be more clinically malignant than oral melanomas and cutaneous melanomas. In veterinary medicine, early enucleation is the treatment of choice for malignant melanocytic tumors and for blind or painful eyes. Postenucleation survival time of 34 cats with diffuse iridial melanoma revealed that cats with advanced cases of intraocular melanoma (infiltration of the iris, its posterior epithelium, ciliary body, and sclera) had a significantly higher risk of developing systemic life-threatening metastases than those with early or moderate infiltration (when neoplastic cells remain confined to the iris stroma and trabecular meshwork (Kalishman et al., 1998; Bourguet et al., 2015). In malignant diffuse iridial melanoma in cats, early enucleation while the tumor is still confined to the iris stroma seems to improve survival time.
ETHICALLY APPROVED
This article does not contain any studies with human participants or experimental animals performed by any of the authors.
ACKNOWLEDGEMENTS
This work was supported by Companion Animal Cancer Research Unit, Department of Pathology, Faculty of Veterinary Science, Chulalongkorn University, Bangkok-10330, Thailand.
CONFLICT OF INTEREST
The authors declare that they have no financial or personal relationship(s) which may have conflicts of interest in writing this article.
AUTHOR’S CONTRIBUTION
All authors contributed equally in all details of this manuscript.
REFERENCES