Advances in Animal and Veterinary Sciences
Case Report
Managing Fetal Mummification in Cows
Viski Fitri Hendrawan1*, Tia Sundari2, Desi Wulansari1, Yudit Oktanella1, Herlina Pratiwi1, Aulia Firmawat1
1Reproduction Department, Faculty of Veterinary Medicine, Brawijaya University, Malang 65151, Indonesia; 2Veterinary Profession Program, Faculty of Veterinary Medicine, Brawijaya University, Malang – 65151, Indonesia.
Abstract | Fetal mummification is a disorder during gestation which happened when fetal death happened in third to eighth month of gestation. This report describes diagnosis and management of several fetal mummification cases in cows in several regions; Mathura, Shimla, Bangladesh, Turkey, Uttarakhand, and Tirupati. Mummification diagnosis is formed by anamnesis, clinical findings, physical examination, rectal palpation, and vaginal palpation. Fetal mummification management was done by analog PGF2α administration and surgical procedures such as episiotomy and Caesarean surgery. Antibiotic was administered in the case of uterine infection.
Keywords | Cow, Diagnosis, Fetus, Management, Mummification
Received | June 25, 2019; Accepted | August 19, 2019; Published | November 01, 2019
*Correspondence | Viski Fitri Hendrawan, Reproduction Department, Faculty of Veterinary Medicine, Brawijaya University, Malang – 65151, Indonesia. Email: viski_hendrawan88@yahoo.com
Citation | Hendrawan VF, Sundari T, Wulansari D, Oktanella Y, Pratiwi H, Firmawat A (2019). Managing fetal mummification in cows. Adv. Anim. Vet. Sci. 7(11): 1006-1009.
DOI | http://dx.doi.org/10.17582/journal.aavs/2019/7.11.1006.1009
ISSN (Online) | 2307-8316; ISSN (Print) | 2309-3331
Copyright © 2019 Hendrawan and Sundari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
Incidence rate of fetal mummification in cows is 0.13-1.8% for cows in gestational period (Kumar and Saxena, 2018). This condition is characterized by decreasing fetal liquid and the presence of brown material surrounding fetus (Kumar et al., 2017). Fetal mummification may happen 3-8 months into gestation (Krishan, 2015; Kumar and Saxena, 2018) after placenta formation and bone formation in fetus, and without cervix dilatation and contamination which caused luteolysis (Kumar and Saxena, 2018). Fetal mummification is followed by persistent corpus luteum, that continue to secrete progesterone (Kumar and Saxena, 2018). The characteristics of fetal mummification is the inability to expulse dead fetus, involution of fetal cotyledon and maternal caruncle, and the presence of hard fetal body within uterine horns without clinical symptoms (Krishan, 2015). In fetal mummification cases caused by non-infectious diseases, hypothesis on the cause intrauterine fetal mummification is fetal dehydration and fetal membrane which neutralize tissue autolysis with the absence of oxygen and bacteria (Kumar and Saxena, 2018). In cow, the most commonly occurring mummification is haematic mummification. Fetal mummification may develop into infection with cervix dilatation and may transform into
fetus maceration (Kumar et al., 2017). Fetal mummification can be treated by administration of prostaglandin 2 or stilbestrol, estradiole, respositol diethylstilbestrol, or by eliminating corpus luteum. If fetal mummification cannot be resolved by the previous treatment, surgical intervention such as Caesarean section (Azizunnesa et al., 2010). Prognosis of mummification cases are good for as long as there is no internal injury to reproductive organ. Fetal mummification may progress into maceration. This may happen caused by failure to abort the fetus and uterine inertia. Bacteria may get into the uterus when cervix dilates and thus a combination of fetal tissue decomposition and autolysis happened and left in the uterus (Noakes, 2001). Every fetal mummification case has different characteristics; thus, this study would discuss how to diagnose and manage various fetal mummification cases.
CASE DESCRIPTION
Comparison of fetal mummification cases in several region is provided in the following table:
Table 1: Fetal mummification cases
| Parameter | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
| (Kumar dan Saxena, 2018) | (Krishan, 2015) | (Azizunnesa et al., 2010) | (Yilmaz et al., 2011) | (Katiyar et al., 2015) |
(Kumar et al., 2017) |
|
| Region | Mathura | Shimla | Bangladesh | Turki | Uttarakhand | Tirupati |
| Breed | - | FH | Sahiwal | FH | Sahiwal | - |
| Number of gestation- | 3 | 1 | 1 | - | 3 | - |
| Age (year) | 6 | 5 | 3,5 | 5 | 6 | 6 |
| Anamnesis | Longer gestation period | Artificially inseminated 310 days before, confirmed pregnant 60-90 days after insemination | In 7 months, mammary and abdomen still developing, 9 months 20 days still no birth | Brown vaginal discharge, inseminated in 196 days before | Longer gestation period, up to 10.5 months | Vaginal discharge, given induction by cloprostenol and diethyl stilbestrol 4 days before |
|
Physical examination (T, HR, RR, Pulsus, gait, BCS, body posture) |
Normal | Normal | Normal | - |
Body temperature 101oF (pyrexia) HR 64 x/minute |
Hyper-thermia, smelly vaginal discharge |
|
Rectal Palpation Compact/firm Fetus Fetal movement Fetal fluid Placentome Fremitus |
Compact None None None |
Compact None None None None |
Compact None None None None |
- |
Uterus contraction around fetus |
Compact None None None None |
|
Vaginal palpation Cervix
Discharge |
Closed
None |
1 finger opening None |
Closed
None |
Opened
Brown |
Closed
None |
Opened
Present |
|
USG Fetal fluid Mass |
None |
- |
- |
None Bone fragment |
- |
- Irregular skeleton, no fetal heart rate
|
|
Treatment
|
Cloprostenol Valethamate bromide Dexamethasone Estradiole Valerate |
Cloprostenol Dicrysticin (antibiotic - 5 days) |
- |
Cloprostenol Ceftiofur hydrochloride (antibiotic - 5 days) |
Cloprostenol Chlorphnira-mine maleat |
Epidosin Oxytocin Did not work |
|
Cervix dilatation (hour) Discharge |
52 | 72-brownish mucoid | - |
36 hours first expulsion. PGF2α was administered again. 58 hours later second expulsion |
48 hours, 2 fingers dilatation, 72 hours opened with vaginal discharge | - |
| Surgery | - | Episiotomy | Left flank caesarean | - | - | Left flank caesarean |
DISCUSSION
Fetal mummification happens sporadically in domestic animal. In cows, hematic mummification often occurs. Etiologically mummification may have infectious or non-infectious causes or may happen in turn or related. Fetal mummification case may be caused by infectious agents such as bovine viral diarrhea, leptospirosis and fungi, and may also by mechanical causes such as umbilical cord torsion, uterine torsion, placentation disorder, genetic abnormalities, and non infectious causes as well as trauma, hyperthermia, and stress (Krishan, 2015). Mummification caused by infectious agent more often happened to small ruminants, dog, and swine compared to horse, cow, and cat (Kumar and Saxena, 2018). However, this does not close the possibility of fetal mummification caused by infectious agent, such as the cases happened in Shimla and Turkey. In this condition, fetal liquid is absorbed, but fetus and membrane are surrounded by brown thick liquid mass. The brown coloration is blood pigment, coming from caruncule hemorrhage caused by fetal death. Umbilical torsion is the primary cause of cow fetal mummification however it is not always found in haematic mummification. Moreover, the condition may occur after estradiol and trembolone acetate hormone induction, which may induce hormonal anomalies, causing the mummification (Noakes, 2001). Prognosis of mummification cases are good for as long as there is no internal injury to reproductive organ. Fetal mummification may progress into maceration. This may happen caused by failure to abort the fetus and uterine inertia. Bacteria may get into the uterus when cervix dilates and thus a combination of fetal tissue decomposition and autolysis happened and left in the uterus (Noakes, 2001).
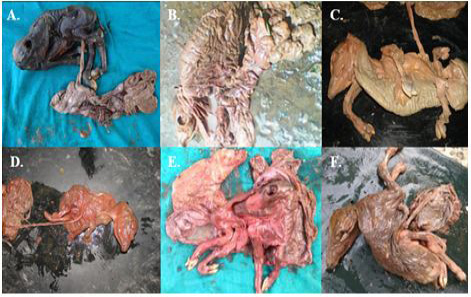
Figure 1: Fetal mummification in respective regions (A. Mathura, B. Shimla, C. Turkey, D. Turkey, E. Uttarakhand, F. Tirupati)
Fetal mummification treatment is by administering PGF2α to regress persistent corpus luteum in the ovary. Estrogen administration may affect CL regression and cause myometrium contraction, cervix relaxation and expulse the mummified fetus in cow (Plumb, 2008). Other research stated that combined administration of PGF2α and estradiol or estrogen gives better result as combined therapy. On the case in Mathura region, prostaglandin, estradiol, valethamate, and costicosteroid combination gave the same effect with physiological partus process in cow. Cervix dilatation occurred with fluid excretion to lubricate genital tract so as to ease the mummified fetus’ path (Kumar and Saxena, 2018). However, the use of estradiol may cause infertility with the residual risk during the administration of the material (Lefebvre et al., 2009). On the case happening in Turkey and Tirupati, the administration of prostaglandin did not manage to induce fetus expulsion, which prompt another administration of prostaglandin or other preparates which can induce uterine contraction such as epidosin which contain valethamate bromide and oxytosin administration. The drug’s mechanism of work is by increasing uterine myofibril permeability which in turn stimulates uterine contraction (Plumb, 2008).
Antibotic administration in fetal mummification cases in Shimla and Turkey was done to prevent uterine infection. They were administered upon the finding of cervix dilatation and murky or brownish discharge, which are indication of bacterial infection (Yilmaz et al., 2011). Without symptoms like pyrexia, toxemia, and infection, antibiotic administrations are not required (Katiyar et al., 2015). Antibiotic such as dicrysticin (penicillin streptomicin) in Shimla region and ceftiofur hydrochloride Turkey region are antibiotics useful for both positive and negative gram, with its mode of action is by inhibiting the synthesis on the hair of peptidoglycan time to phone (Plumb, 2008).
Other than utilizing drugs, fetal mummification may also be resolved with surgery or a combination of the true. Surgical procedure such as hysterotomy has several advantages and disadvantages for fetus mummification treatment. Hysterotomy advantage is the ease of taking out fetus however the disadvantages is the long recovery period and the risk of uterine unable to conceive again. In cases like Shimla region, fetus was big and difficult to drag out, and thus treated by episiotomy to enlarge fetus’s route. In case like Bangladesh region, fetal mummification prompts swift surgical procedur, while in Tirupati, drugs that did not cause induction was then overthrown by the government to proceed to surgical procedures.
Anesthetic used for surgical procedures are local anesthetic. Episiotomy was done by injecting lidocaine 2% around vulva while caesarean surgery was done by injecting lidocaine 2% and diazepam into paravertebral region. Incision was done on left flank. Peritoneum in lavage used normal saline and metronidazole liquid into the abdomen to eliminate infectious agent contamination. During and after surgery, fluid therapy was administered according to cow’s condition. Antibiotic and analgesic were given post surgery along with treatment for the surgical wound (Kumar et al., 2017).
Based on previous fetal mummification cases, mummification case management in Mathura can be seen as a reference for non-surgical surgical procedure, however the drug mode of action used is imitating normal fetal passing. Mummification case in Tirupati can become the references as treatment by surgery. This was taken after prostaglandin drugs inductions were unable to open the cervix and expulse the fetus.
CONCLUSION
Fetal mummification management is divided into surgical and non-surgical procedure. The use of drugs (non-surgical procedure) such as prostaglandin are the safer approach and in line with the natural mechanism of fetus delivery, like the case in Mathura region. Surgical procedure in the form of flank Caesarean section is conducted if the use of drugs could not deliver the fetus out, just like what occurred in Tirupati case.
ACKNOWLEDGEMENT
The authors would like to thank Faculty of Veterinary Medicine, Brawijaya University, for providing all supporting facilities.
CONFLICT OF INTEREST
No conflict of interest to declare.
REFERENCES







